Pharmacogenomics: How Your Genes Affect Medication Response
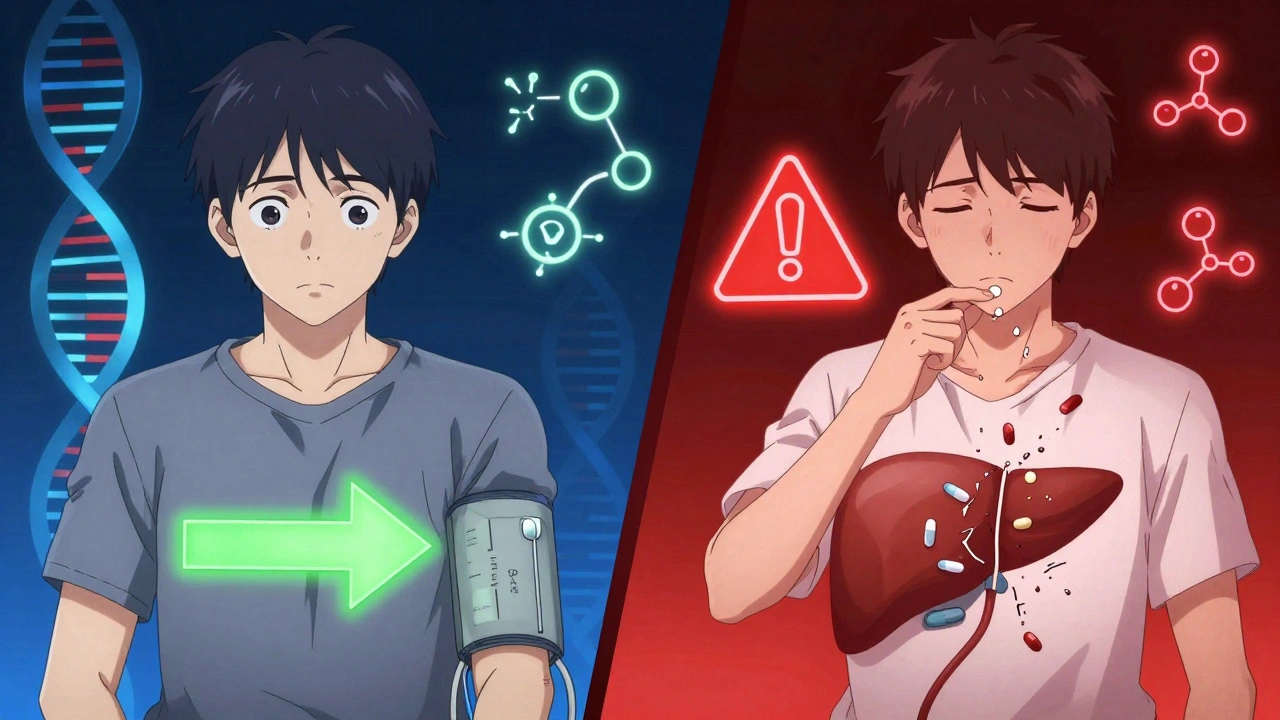
When you take a pill, your body doesn’t just react the same way everyone else does. Your genes play a big role in how fast you break down drugs, whether you get side effects, or if the medicine even works at all. This is pharmacogenomics, the study of how your genetic makeup affects your response to medications. Also known as personalized medicine, it’s not science fiction—it’s already changing how doctors choose your prescriptions.
Take statins for cholesterol. Some people get muscle pain from them. Others don’t. Why? It’s often because of a gene called SLCO1B1. If you have a certain version of it, your body can’t clear the drug properly, and toxicity builds up. Same with warfarin, the blood thinner. A tiny difference in two genes—CYP2C9 and VKORC1—can mean the difference between a safe dose and a dangerous one. That’s why some hospitals now test patients before prescribing. It’s not about guessing anymore. It’s about knowing.
And it’s not just about avoiding bad reactions. Pharmacogenomics helps doctors pick the right drug the first time. For example, if you have depression and tried two antidepressants that didn’t work, your doctor might check your CYP2D6 gene. That gene tells them if you’re a slow, normal, or fast metabolizer. Slow metabolizers might need lower doses. Fast ones might need stronger ones. This isn’t rare. About 90% of people have at least one genetic variation that affects how they handle common meds. The drug metabolism, the process your liver uses to break down medications is heavily influenced by your DNA. And that’s where genetic testing, a simple cheek swab or blood test that looks at key drug-response genes comes in. It’s becoming faster, cheaper, and more common—even in primary care.
You won’t find a single test that covers everything. But for key drugs—antidepressants, blood thinners, pain meds, and cancer treatments—genetic info is already guiding decisions. It’s part of why some people get lucky with their meds and others don’t. It’s not about being weak or strong. It’s about biology. And now, we’re starting to listen to your genes.
Below, you’ll find real-world guides on how drugs behave in your body, what causes side effects, how liver function changes things, and why some meds interact dangerously with food or other pills. These aren’t abstract ideas. They’re the practical side of pharmacogenomics—what happens when genes meet prescriptions.
Ethnicity influences how your body processes medications due to genetic differences in drug metabolism. Learn how CYP450 enzymes, HLA variants, and pharmacogenomics are changing prescribing practices to improve safety and effectiveness.