Global Health Economics: How Money, Policy, and Medicines Shape Your Care
When we talk about global health economics, the study of how resources are allocated to improve health outcomes across countries. It's not just about hospitals and pills—it's about who gets treated, who doesn't, and why some medicines cost ten times more in one country than another. This isn't abstract theory. It's the reason a life-saving HIV drug might be unreachable in rural Africa while sitting in a warehouse in the U.S., or why a generic version of a common antibiotic is now the default in workers' compensation programs across most U.S. states.
medication rationing, the process of deciding who receives limited drugs during shortages is one of the most painful outcomes of broken health economics. When supplies run low, hospitals don't flip coins—they use ethical frameworks to prioritize patients based on need, survival chances, and fairness. This happens more often than you think. Drug shortages aren't rare emergencies; they're systemic failures tied to manufacturing, pricing, and global supply chains. And when those chains break, it's not just hospitals that suffer—it's the people waiting for their next dose of insulin, chemotherapy, or antibiotics.
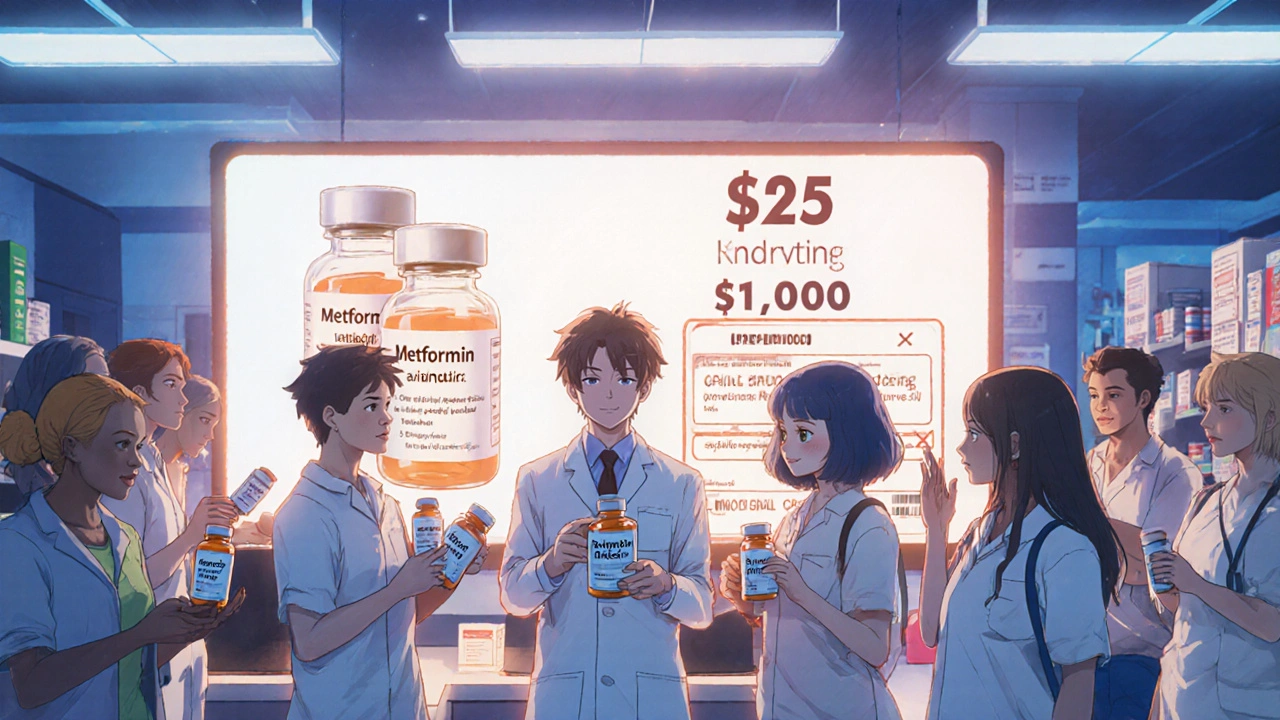
generic drugs, FDA-approved copies of brand-name medicines that cost far less are the quiet heroes of global health economics. They make up over 90% of U.S. prescriptions today, saving billions every year. But their rise didn’t happen by accident. It was driven by laws like the Hatch-Waxman Act, which balanced innovation with access. Yet even generics face barriers—patent tricks, supply bottlenecks, and price gouging in places without strong regulation. In some countries, a generic version of a drug costs pennies. In others, it’s still out of reach.
Then there’s healthcare ethics, the moral framework guiding who gets care when resources are scarce. Should a young patient with a higher chance of recovery get priority over an older one? Should a worker injured on the job get cheaper generics while a private patient pays full price? These aren’t hypotheticals—they’re daily decisions made in ERs, clinics, and policy rooms. And they’re all shaped by the same invisible force: global health economics.
You’ll find real stories here: how drug shortages force hospitals to choose who lives, how generic substitution cuts costs without cutting care, how pricing policies make some medicines unaffordable even when they’re made in the same country. These aren’t distant policy debates. They’re the reason your neighbor can’t refill their prescription, why your doctor switches your medication without asking, and why some treatments are still out of reach for millions.
Generics are the backbone of affordable global healthcare, saving trillions while 37 countries cut spending. Discover how low-cost drugs keep millions alive - and why they're under threat.