When you pick up a prescription, you might not realize you have options that could cut your cost by half-or even 90%. The key isn’t just getting any generic drug. It’s knowing whether you’re getting a generic or an authorized generic, and how your insurance treats each one. Most people don’t ask. But if you ask the right questions, you could save hundreds a year.
What’s the Difference Between Generic and Authorized Generic Drugs?
Generic drugs are FDA-approved copies of brand-name medications. They contain the same active ingredients, work the same way, and must meet strict bioequivalence standards. That means your body absorbs them just like the brand-name version. The FDA requires generics to be within 80-125% of the brand’s absorption rate-so they’re not just similar, they’re clinically identical. Authorized generics are different. They’re made by the same company that produces the brand-name drug, often in the same factory, using the exact same formula. But instead of being sold under the brand name, they’re labeled as generics. Think of it like a car manufacturer selling the same model under a different badge. The product is unchanged, but the price drops because it’s marketed as a generic. Here’s why it matters: brand-name companies often launch authorized generics right after their patent expires. This lets them keep some market share while still lowering prices. But because they’re made by the original manufacturer, they sometimes don’t trigger the same insurance discounts as traditional generics.How Much Can You Really Save?
The numbers speak for themselves. In 2022 alone, generic and biosimilar drugs saved the U.S. healthcare system over $408 billion. Over the last decade, that total hit $2.9 trillion. Most of that savings comes from price drops after generic entry. Within a year of a generic version launching, prices typically fall by more than 75%. In some cases-like the diabetes drug Truvada-prices dropped from $50 per pill to under $3. That’s a 94% reduction. The FDA found that 77 drugs saw price cuts of over 90% in the first year after generic approval. But here’s the catch: list price and what you pay at the pharmacy aren’t always the same. Insurance formularies and pharmacy benefit managers (PBMs) decide how much you pay out of pocket. One 2023 study found that patients who asked specifically about authorized generics saved 15-25% more than those who just asked for “a generic.”Why Your Copay Might Not Drop Even When the Price Does
You might think: “If the drug costs less, my copay should too.” Not always. Many insurance plans treat authorized generics differently than traditional generics. Some put them on the same tier as brand-name drugs. Others give them better coverage. It depends on your plan’s contract with the PBM. One patient on Reddit shared: “My insulin went from $350 brand to $90 authorized generic-but my copay stayed at $45.” Why? Because their plan didn’t recognize the AG as a lower-tier drug. Meanwhile, another user switched from an authorized generic to a traditional generic for their blood pressure medication and saved $20 a month-even though both drugs were chemically identical. The reason? Traditional generics often come with aggressive rebate deals between manufacturers and PBMs. Authorized generics sometimes don’t participate in those deals, so insurers don’t pass along the savings.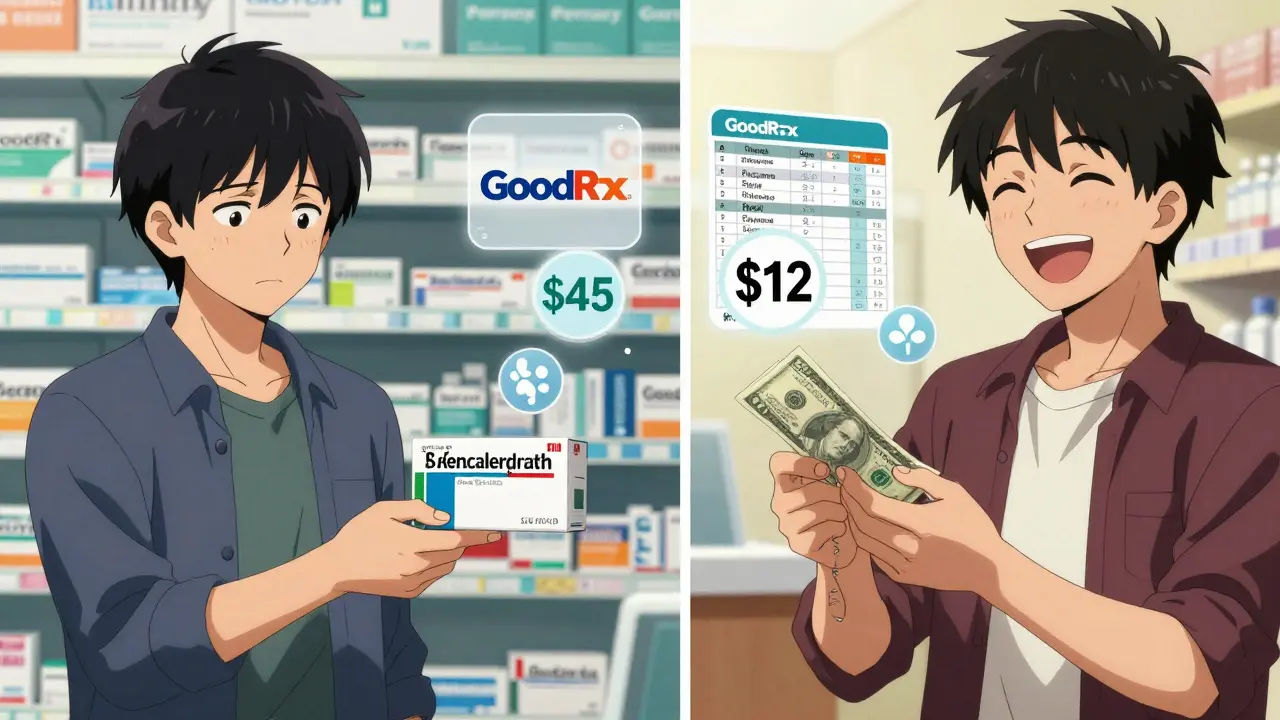
What to Ask Your Pharmacist (And How to Ask It)
Don’t just say, “Do you have a generic?” That’s too vague. You need to ask targeted questions. Here’s what to say:- “Is there a generic version of this drug available?” - This starts the conversation.
- “Is this an authorized generic?” - If they say yes, ask follow-up questions.
- “How does my insurance treat authorized generics versus traditional generics?” - This forces them to check your plan’s formulary.
- “Can I switch between generic types to save money?” - Sometimes, a traditional generic costs less even if the AG is cheaper on paper.
Use Tools to Compare Cash Prices
Insurance isn’t the only factor. Sometimes, paying cash is cheaper than using your copay. Apps like GoodRx and SingleCare show cash prices for both traditional and authorized generics at nearby pharmacies. You might find that the cash price of a traditional generic is lower than your copay for the authorized version. For example: Your copay for an authorized generic is $40, but the cash price for a traditional generic at Walmart is $12. That’s not a typo. It happens often with older, high-volume drugs like metformin or lisinopril. Always check both options. Even if you have insurance, paying cash might still be smarter.Which Drugs Have the Biggest Savings?
Not all drugs drop in price the same way. Some categories see massive savings; others don’t.- Cardiovascular drugs - 98% of prescriptions are filled with generics. Savings are huge. Drugs like atorvastatin (Lipitor) and metoprolol (Lopressor) cost 90% less than brand versions.
- Diabetes medications - Insulin generics are still emerging, but authorized generics have cut prices by 60-80% for many patients.
- Antibiotics and blood pressure meds - Often under $5 for a 30-day supply as generics.
- Specialty drugs - Things like injectables, inhalers, or skin creams have fewer generics. The FDA reports that only 60% of specialty prescriptions use generics, even after patents expire.
What’s Changing in 2026?
The FDA’s 2023 Drug Competition Action Plan is targeting hard-to-copy drugs like inhalers, topical creams, and complex injectables. They’re streamlining approval to bring down prices faster. Biosimilars (generic versions of biologic drugs like Humira or Enbrel) are also growing. Over 30 have been approved, and they’re priced, on average, 50% below the brand. Savings from biosimilars hit $7 billion in 2023. But challenges remain. Drug shortages hit 307 in 2022. Manufacturing is concentrated in just a few countries. And some companies still use “patent thickets” - filing dozens of minor patents to block generics. Still, the trend is clear: generics work. And if you know how to ask for them, you’ll pay less.Real-World Tip: The 2-Minute Prescription Check
Before you leave the pharmacy, do this:- Ask: “Is this an authorized generic?”
- Ask: “What’s the cash price for the traditional generic?”
- Check GoodRx on your phone while you wait.
- If cash is cheaper than your copay, ask if you can pay cash instead.
Are authorized generics as safe as traditional generics?
Yes. Both authorized generics and traditional generics must meet the same FDA standards for safety, strength, quality, and performance. Authorized generics are made by the original brand manufacturer using the same formula and facilities. The only difference is how they’re labeled and priced. You’re getting the exact same medicine.
Why do some generics cost more than others even if they’re the same drug?
It’s about insurance contracts. Different manufacturers negotiate different rebates with pharmacy benefit managers (PBMs). One generic might have a $5 copay because the manufacturer gave a big rebate. Another might cost $20 because it didn’t. The drug is identical, but your plan’s deal with the maker changes your out-of-pocket cost.
Can I ask my doctor to prescribe a generic instead of a brand?
Absolutely. Most doctors default to brand names because that’s what they’re taught. But you can say: “Is there a generic version of this? Could you prescribe it instead?” Many doctors will switch without question-especially for common drugs like statins, blood pressure meds, or antidepressants.
Do authorized generics delay cheaper generics from entering the market?
Sometimes, yes. When a brand company launches its own authorized generic, it can block other manufacturers from entering. This happened with drugs like Humira and Epclusa. The brand company gets to keep profits while still offering a “generic” label. Experts say this practice is declining, but it still happens-and it can delay savings for patients.
Is it worth switching from a brand-name drug to a generic?
For almost everyone, yes. The FDA requires generics to perform the same as brand-name drugs. Studies show no difference in effectiveness or side effects. The only reason not to switch is if you’ve had a rare reaction to a specific generic manufacturer-something that happens in less than 1% of cases. If you’re unsure, ask your pharmacist or doctor.


12 Comments
Brad RalphFebruary 12, 2026 AT 17:22
Yup. Just asked for a generic at CVS yesterday. Got an authorized one. Copay was $42. Walked to Walmart, paid $8 cash. Mind blown. 🤯Annie JoyceFebruary 12, 2026 AT 23:22
I work in pharmacy tech and this is wild how few people ask. Last week a guy got prescribed lisinopril, asked for generic, got the authorized one for $38. I showed him the $5 cash price on GoodRx. He nearly cried. We need a public service campaign. Seriously. People are getting ripped off daily and don't even know it.Vamsi KrishnaFebruary 13, 2026 AT 08:05
LMAO you guys think this is new? I've been doing this since 2018 when I was on insulin. Authorized generics are a scam dressed in FDA clothes. The brand company still owns the damn thing, just slaps a 'generic' label on it to keep the PBM rebate money for themselves. Meanwhile, real generics? Those are the ones made by Indian manufacturers who don't play ball with PBMs. That's where the real savings are. Stop being fooled by marketing. Ask for the *real* generic. Not the one that looks like a generic but still has the brand's fingerprints all over it.Sophia NelsonFebruary 14, 2026 AT 07:44
I tried this. Asked for a generic. Got an authorized one. Paid $45. Then I went to another pharmacy. Same drug. Cash price $14. They didn't even ask if I had insurance. Just handed it over. I felt like a genius. Also, why do pharmacists act like I'm asking for a moon landing when I say 'authorized generic'?Carla McKinneyFebruary 15, 2026 AT 22:07
This is why I stopped trusting the system. The FDA says they're equivalent. But if they're equivalent, why does my insurance treat them differently? Why does one version get a $5 copay and another get $35? It's not about efficacy. It's about corporate contracts. You're not saving money because you're smart. You're saving money because you're playing a rigged game. And the only people who win are the PBMs and the manufacturers who negotiated the best deals. You're just a pawn.Reggie McIntyreFebruary 16, 2026 AT 15:28
I just switched my dad from brand-name metformin to a traditional generic after reading this. His monthly bill dropped from $120 to $4. He’s been on it for 12 years and never knew this was possible. I cried. Not because it’s sad. Because it’s absurd. We’re paying $120 for a pill that costs $0.40 to make. And no one told us. This isn’t healthcare. It’s a hostage situation.andres azFebruary 17, 2026 AT 05:01
You think this is about savings? Nah. This is about control. The FDA, PBMs, and Big Pharma are all in cahoots. Authorized generics? They're a Trojan horse. They let the original manufacturer keep market share while pretending to be 'competitive'. Meanwhile, real generics get stuck in supply chain purgatory because they're made overseas. And guess who gets to decide which pharmacy gets which drug? The PBM. You think you're saving money? You're just being steered toward the option that gives the middlemen the biggest cut. Wake up.Stephon DevereuxFebruary 17, 2026 AT 13:43
This changed my life. I used to pay $200/month for my blood pressure med. After asking the right questions, I found out the authorized generic was $85. Then I checked GoodRx. The traditional generic? $12. I switched. My pharmacist was stunned. Said he'd never seen someone do the legwork. Now I do this for every prescription. I'm not rich. I'm just curious. And curiosity saves money. Don't let fear or laziness cost you thousands a year. You're worth the two minutes.steve sunioFebruary 19, 2026 AT 04:41
i hve been doin this since 2020. its all about the pmb. the real genric is always cheaper. but most pharms dont tell u. they want u to use the ins. so they get the cut. i pay cash for everything now. even if i have ins. its cheaper. and dont get me started on authorized generics. its just brand name with a fake label. lolJoanne TanFebruary 19, 2026 AT 12:41
I did the 2-minute check yesterday on my antidepressant. Authorized generic: $38 copay. Traditional generic cash price: $7. I paid cash. Felt like I won the lottery. Also, my pharmacist smiled for the first time since I've been going there. She said, 'I wish more people did this.' Honestly? This should be taught in high school. Like, next to sex ed and taxes.Jack HavardFebruary 20, 2026 AT 20:36
The whole system is designed to confuse you. They want you to think 'generic = cheap' and 'authorized = better.' But it's the opposite. Authorized generics are the expensive version of cheap. The real savings come from generics made by companies that don't have contracts with PBMs. The FDA doesn't care about your wallet. They care about bioequivalence. You? You care about your rent. So stop trusting the labels. Trust the cash price.Suzette SmithFebruary 22, 2026 AT 16:17
Actually, I think you're wrong. I switched from a traditional generic to an authorized one last month because my insurance started covering it better. I went from $18 to $12. So sometimes, the authorized one wins. Not always. But sometimes. Don't demonize it.