Every year, the world spends more on healthcare than the last. But not all of that money goes to fancy new drugs. In fact, a huge chunk of what keeps people alive and healthy comes from something simple, cheap, and often overlooked: generics.
Why Generics Matter More Than You Think
When you walk into a pharmacy and pick up a bottle of metformin for diabetes or amoxicillin for an infection, there’s a good chance it’s not made by Pfizer or Merck. It’s probably made by a company in India, China, or Eastern Europe - and it costs a fraction of the brand-name version. That’s a generic drug. And globally, these low-cost versions make up 80-90% of all prescriptions filled in high-income countries.
But here’s the catch: even though generics are everywhere, they’re not equally available everywhere. In the United States, where drug spending hit $487 billion in 2024, generics helped hold down costs. Without them, that number could have been $200 billion higher. In contrast, in countries like Nigeria, Afghanistan, or Turkmenistan, most people pay for medicine out of their own pockets - and often can’t afford even the generic versions. In those places, generics aren’t a cost-saving tool; they’re a luxury.
The Numbers Behind Global Healthcare Spending
By 2025, the world will spend about $1.6 trillion on medicines. That’s a lot - but it’s not growing evenly. The biggest driver? New, expensive drugs for cancer, autoimmune diseases, obesity, and diabetes. These aren’t generics. These are patents held by big pharma companies, priced to recoup billions in R&D. In the U.S. alone, drug spending is projected to nearly double from $776 billion in 2025 to $1.7 trillion by 2033.
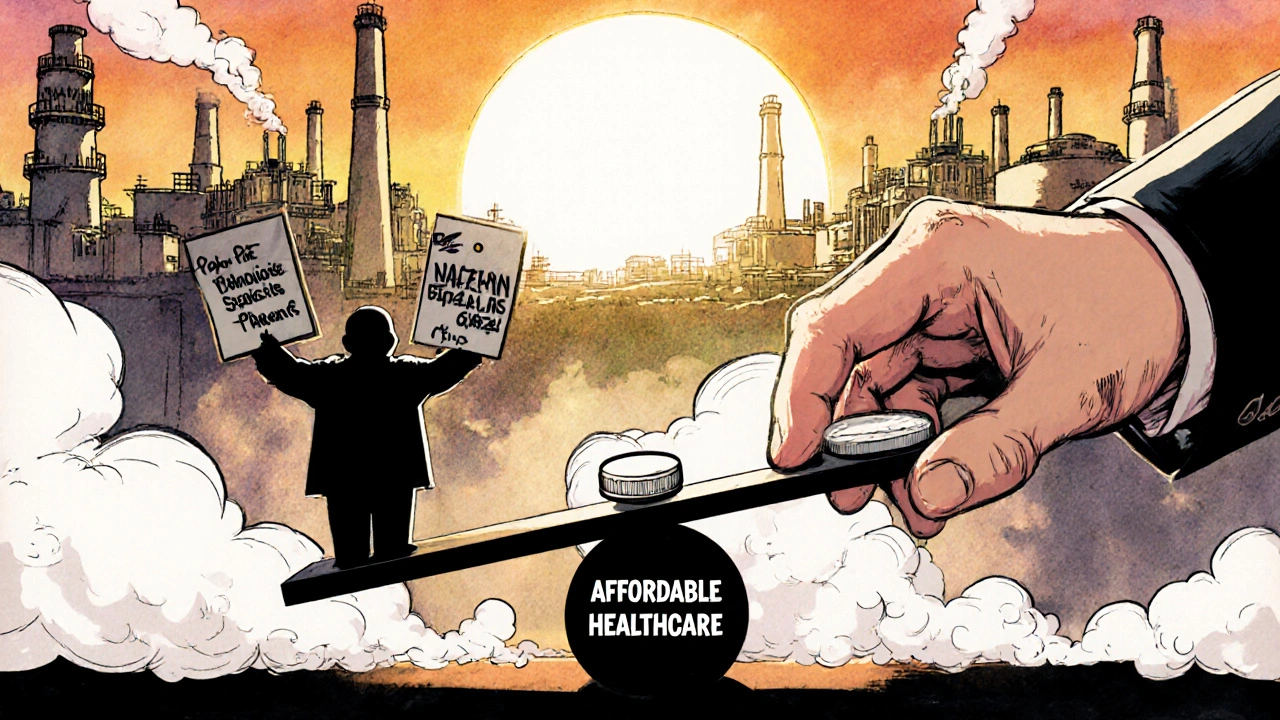
Meanwhile, public healthcare spending globally averages just 3.8% of GDP. That’s not enough. In low-income countries, it’s as low as 1.2%. In high-income countries, it’s 5.8%. The gap isn’t just about money - it’s about survival. Thirty-seven countries saw their real healthcare spending drop after the pandemic. Lebanon lost 71%. Malawi lost 41%. In places like that, every dollar counts. And generics are the only thing standing between people and untreated illness.
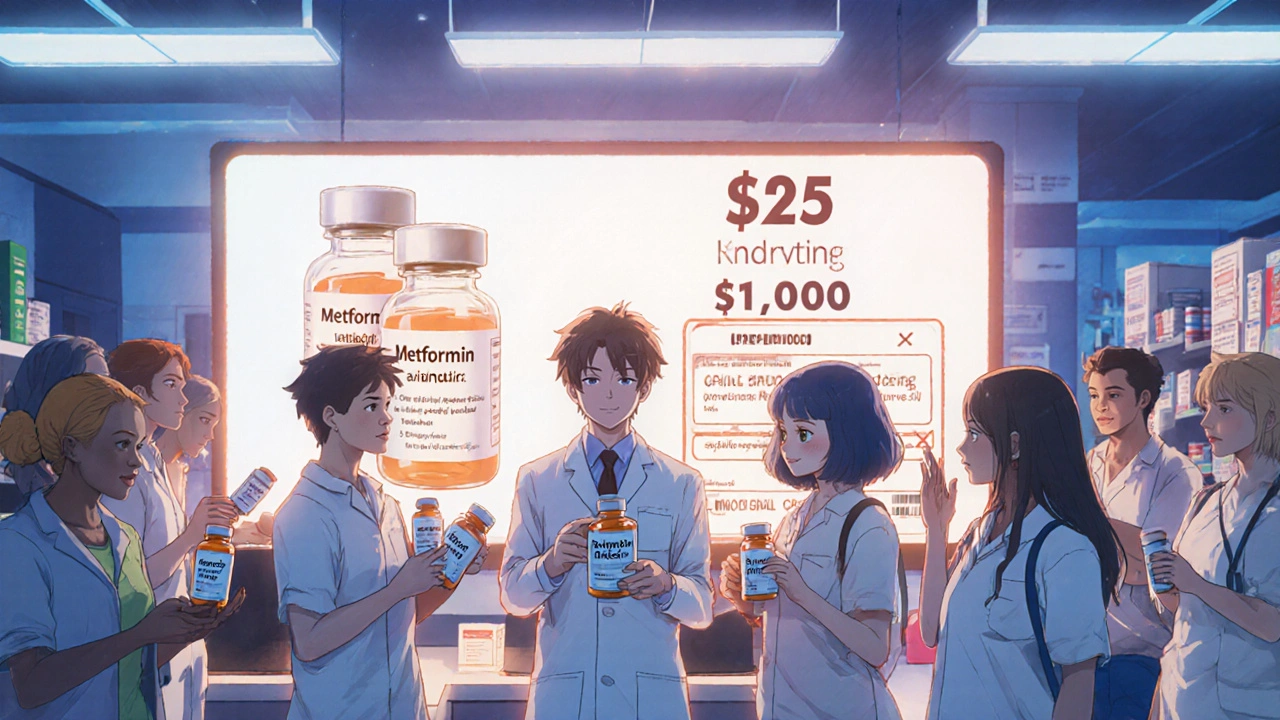
How Generics Keep Costs Down - and Where They Can’t
Generics don’t just save money. They change behavior. When a brand-name drug loses its patent, prices typically drop by 80-95%. That’s why insulin, once priced at $1,000 per vial, can now be bought for under $25 in generic form in some countries. But not all drugs have generics. Biologics - complex drugs made from living cells - are harder to copy. Their cheaper versions, called biosimilars, are still rare outside of Europe and North America. In the U.S., only a handful of biosimilars have entered the market, and doctors are slow to switch. In Africa and Asia, they’re almost nonexistent.
That’s a problem. Oncology, immunology, and mental health drugs are among the fastest-growing spending categories. In the U.S., out-of-pocket costs for prescriptions are set to rise 30.5% by 2033. Mental health drugs alone? Insurers expect demand to jump 15% or more in the next three years. If we don’t expand access to affordable versions of these drugs, millions will be priced out.

Where Generics Are Winning - and Losing
Europe and Latin America are seeing medical cost growth slow down. Why? Strong generic substitution policies. In the UK, Germany, and Spain, pharmacists can automatically swap brand drugs for generics unless the doctor says no. That’s not the case in the U.S., where doctors often prescribe by brand name, and patients assume the name-brand version is better.
Meanwhile, countries like China are shifting away from generics. As incomes rise and healthcare systems expand, China is importing more expensive, innovative drugs. It’s a sign of progress - but also a warning. When a country moves from generic-heavy to brand-heavy, spending spikes. And if that happens in India or Brazil, the global balance could tip.
Insurers are watching closely. Two-thirds say the cost of new medical tech is their biggest worry. In the Americas, 88% blame new technologies. In Asia Pacific, it’s 73%. That means generics aren’t just about saving money - they’re the only tool left to stop healthcare from becoming unaffordable for everyone.
The Hidden Cost of Not Using Generics
Think about this: if you’re a family in Nigeria paying $50 out of pocket for a monthly hypertension drug, and the generic costs $2, you’re spending 10% of your monthly income just to stay alive. That’s not healthcare. That’s financial ruin.
And it’s not just poor countries. In the U.S., 25% of adults skip doses because they can’t afford their meds. Even with insurance, co-pays for brand-name drugs can hit $100 a month. Generics cut that to $5. That’s not a small difference. It’s the difference between treatment and no treatment.
Global health aid is shrinking too. In 2025, development assistance for health will drop to $39.1 billion - the lowest since 2009. That means governments and NGOs can’t fill the gap. Generics are the only scalable solution.
The Future of Generics: More Than Just Cheap Pills
The next decade won’t be about whether generics matter. It’ll be about how we make them work better. Regulatory delays, patent evergreening, and lack of competition in some markets are holding back access. In the U.S., some generic manufacturers have been accused of colluding to keep prices high. In India, export restrictions during the pandemic exposed how fragile the supply chain is.
But there’s hope. Countries like Canada, Australia, and the UK are pushing for faster approval of generics. The WHO is pushing for bulk purchasing agreements. And new technologies - like AI-driven manufacturing - could make generics even cheaper and more reliable.
What’s clear is this: if we want to control healthcare spending, we can’t just rely on new drugs. We need to invest in the old ones - the ones that work, that are safe, and that cost pennies. Generics aren’t the future of healthcare. They’re the foundation.
What You Can Do - Even If You’re Not a Policymaker
You don’t need to be a government official to make a difference. When your doctor writes a prescription, ask: "Is there a generic version?" If your pharmacy doesn’t offer it, ask why. If your insurance won’t cover it, call them. Demand transparency.
Support policies that allow pharmacists to substitute generics automatically. Push for bulk purchasing in your community. And if you’re in a country with access to generics, don’t take them for granted. They’re the reason millions can afford to live.
Why are generic drugs so much cheaper than brand-name drugs?
Generic drugs cost less because they don’t require the same research, development, and marketing expenses as brand-name drugs. Once a patent expires, other manufacturers can produce the same active ingredient without repeating costly clinical trials. They only need to prove their version is bioequivalent - meaning it works the same way in the body. That cuts costs dramatically, often by 80-95%.
Do generics work as well as brand-name drugs?
Yes. By law, generics must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict quality standards set by regulators like the FDA or EMA. Studies consistently show they are equally effective and safe. The only differences are in inactive ingredients - like color or filler - which don’t affect how the drug works.
Why aren’t generics available for all drugs?
Some drugs, especially biologics like insulin, Humira, or Enbrel, are made from living cells and are extremely complex to replicate. Their cheaper versions, called biosimilars, take longer to develop and face stricter regulatory hurdles. Also, some drugmakers extend patents through minor changes - a practice called "evergreening" - which delays generic entry. In some countries, legal or regulatory barriers also slow down approval.
How do generics affect healthcare systems in poor countries?
In low-income countries, generics are often the only way people can access life-saving medicines. Without them, diseases like HIV, malaria, and tuberculosis would be untreatable for most. Organizations like the Global Fund and WHO rely heavily on bulk-purchased generics to provide treatment at scale. When generics are unavailable or too expensive, treatment coverage drops - and deaths rise.
Is the global supply of generics reliable?
It’s mixed. India and China produce over 80% of the world’s generic drugs, making the supply chain vulnerable to export bans, trade disputes, or natural disasters. During the pandemic, shortages of generic antibiotics and anesthetics showed how fragile this system is. But efforts are growing to diversify production - with manufacturers in Brazil, Egypt, and Vietnam stepping up. Still, more investment in local manufacturing is needed to ensure stability.
Why do some doctors still prescribe brand-name drugs over generics?
Some doctors are used to prescribing by brand name, especially if they were trained that way. Others worry patients will think generics are inferior - even though that’s not true. Pharmaceutical marketing also plays a role: reps visit doctors with free samples of brand-name drugs, creating habits that are hard to break. In places like the U.S., where patients often expect the name-brand version, doctors may prescribe it to avoid complaints.
Can generics help reduce out-of-pocket costs for patients?
Absolutely. In the U.S., out-of-pocket spending on prescriptions is projected to rise from $177 per person in 2025 to $231 by 2033. Switching to generics can cut that cost by 90% for many drugs. For someone taking multiple medications, that could mean saving hundreds - or even thousands - of dollars a year. In countries without insurance, generics are often the only affordable option.
Are biosimilars the same as generics?
Not exactly. Biosimilars are the generic-like versions of biologic drugs - complex medicines made from living organisms. Unlike traditional generics, which are exact copies of small-molecule drugs, biosimilars are highly similar but not identical. They require more testing and are more expensive to produce. Still, they’re significantly cheaper than the original biologics and are crucial for making treatments like cancer therapies more affordable.
What’s stopping more countries from using generics?
Several things: weak regulatory systems, lack of awareness among doctors and patients, patent protections, and pharmaceutical lobbying. In some countries, doctors aren’t trained to prescribe generics. In others, pharmacies don’t stock them because they make less profit. And in places with high out-of-pocket spending, patients may not know generics exist - or think they’re "inferior" because they’re cheaper.
Will generics continue to be important in the future?
More than ever. As drug prices keep rising and healthcare systems strain under financial pressure, generics are the most scalable solution. Even as new drugs emerge, the world still needs affordable options for chronic conditions like hypertension, diabetes, and depression. Without generics, millions will be left behind. Their role isn’t fading - it’s becoming more critical.

11 Comments
Paige LundNovember 19, 2025 AT 11:45
Wow. Another essay on generics. Can we just get a meme next time?
Reema Al-ZaheriNovember 19, 2025 AT 23:11
Generics are not merely "cheap pills"-they are the structural backbone of equitable healthcare access in resource-constrained environments. In India, where over 70% of prescriptions are filled with generics, the public health infrastructure relies on their consistent availability, affordability, and regulatory compliance. Yet, despite this, supply-chain fragility, patent evergreening, and lack of physician education continue to undermine their potential. The real crisis isn’t the cost-it’s the systemic neglect of distribution, awareness, and policy enforcement.
Codie WagersNovember 20, 2025 AT 22:34
You speak of generics as if they’re some moral imperative-yet you ignore the truth: medicine isn’t charity. It’s a market. Companies don’t develop drugs out of altruism; they do it for profit. Generics don’t "save lives"-they exploit the labor of researchers who bore the risk. The real tragedy isn’t that generics exist-it’s that we’ve normalized the idea that life-saving treatment should be a commodity, not a right. And now we’re surprised when people can’t afford it? Pathetic.
Let’s stop pretending this is about access. It’s about power. Who controls the molecule? Who owns the patent? Who decides who lives and who dies? Generics are a Band-Aid on a severed artery.
Richard RisembergNovember 22, 2025 AT 12:11
Let me tell you something real: I used to be one of those people who thought brand-name was better-until my kid got asthma and we couldn’t afford the inhaler. Then we tried the generic. Same box. Same instructions. Same results. No magic. No placebo. Just a $5 vial instead of $120. That’s not a win for capitalism-that’s a win for human decency. And if you’re still skeptical, go ask a single mom in rural Alabama who’s skipping meals to pay for her insulin. She’ll tell you what ‘equivalent’ really means.
Generics aren’t just cheap-they’re courageous. They’re the quiet heroes in the back of the pharmacy shelf. Let’s stop talking about them like they’re second-rate. They’re the reason millions aren’t dead.
Andrew MontandonNovember 24, 2025 AT 01:27
Y’ALL. I just found out my blood pressure med is generic-and I’ve been paying $90 a month for it. Turns out? The same pill is $4 at Walmart. FOUR DOLLARS. I’m not mad-I’m furious. Why didn’t anyone tell me? Why does the system make us feel guilty for asking if there’s a cheaper version? This isn’t rocket science. It’s pharmacy 101. If you’re paying full price for a generic, you’re being scammed. And if your doctor won’t write for it? Fire them. Seriously. We need to stop normalizing financial abuse in healthcare.
Sam ReicksNovember 24, 2025 AT 16:19
u think generics are safe but what if the fda is in on it and the pills are laced with microchips to track your health habits and sell data to big pharma they make you think its cheap but its actually part of a global surveillance op and the real drugs are only available in secret underground labs in switzerland no one talks about this but my cousin works at a compounding pharmacy and he says the real stuff glows under uv light and tastes like metal and no one wants to admit it but the government wants you dependent on the cheap stuff so you dont rebelFrank DahlmeyerNovember 25, 2025 AT 03:02
Consider the broader context: the global pharmaceutical industry is a $1.4 trillion behemoth, and while generics account for 80% of prescriptions, they generate less than 20% of revenue. Why? Because the margins are razor-thin. Manufacturers operate on thin margins, often in regions with lax labor and environmental regulations. Meanwhile, the same companies that produce generics are often subsidiaries of the very firms that hold the patents on the original drugs. So when we celebrate generics as a victory for affordability, we’re celebrating a corporate strategy that allows one entity to profit twice-once from the high-price brand, then again from the low-price generic. It’s not a system designed for equity. It’s a system designed for extraction, repackaged as compassion.
And let’s not forget: the real innovation isn’t in the pill-it’s in the marketing. The branding, the packaging, the doctor incentives, the patient education campaigns that make people believe the blue pill is better than the white one. We’ve been conditioned to equate price with quality. That’s not science. That’s psychology. And it’s killing people.
Dion HetemiNovember 25, 2025 AT 08:06
Let’s be brutally honest: the entire generics narrative is a distraction. While we’re arguing over $5 insulin, the real cost drivers are hospital administration, insurance overhead, and the $200 billion spent annually on direct-to-consumer drug ads. Generics help, sure-but they’re not the solution. They’re a Band-Aid on a hemorrhage. We’re fixing the wrong problem while the system bleeds out. Until we break the monopoly on drug pricing and end the FDA’s slow-approval trap, we’re just rearranging deck chairs on the Titanic.
And don’t even get me started on how insurers still refuse to cover biosimilars unless you’ve tried and failed five brand-name drugs first. That’s not healthcare. That’s torture.
Kara BinningNovember 26, 2025 AT 01:01
AMERICA IS THE ONLY COUNTRY THAT LETS PHARMA COMPANIES CHARGE WHAT THEY WANT. IN CANADA, THE UK, GERMANY-GENERIC DRUGS ARE CHEAP BECAUSE THE GOVERNMENT SETS THE PRICE. HERE? WE LET CORPORATIONS ROB PEOPLE. I’M NOT SAYING WE NEED SOCIALISM-I’M SAYING WE NEED TO STOP BEING NAIVE. IF YOU THINK THIS SYSTEM IS FAIR, YOU’VE NEVER HAD TO CHOOSE BETWEEN MEDS AND RENT. THIS ISN’T A POLICY ISSUE. IT’S A MORAL CRIME.
Michael PeteschNovember 26, 2025 AT 01:31
As a medical anthropologist who has worked across seven low-income nations, I can confirm: the absence of accessible generics is not merely an economic failure-it is a cultural one. In many communities, the perception of pharmaceuticals is deeply tied to visual cues: color, shape, branding. A white tablet with no logo is perceived as ineffective, regardless of bioequivalence. This is not ignorance-it is the legacy of decades of targeted marketing that equated foreign packaging with quality. Until we address this psychological barrier-through community health workers, culturally competent education, and local manufacturing that preserves familiar aesthetics-we will continue to see treatment abandonment, even when the medicine is available.
Generics are not just pills. They are symbols. And we must learn to redesign the symbol before we can change the outcome.
Angela GutschwagerNovember 27, 2025 AT 19:43
Just ask for the generic. It’s that simple. 😌