Every year, millions of people in the U.S. and UK take SSRIs to manage depression, anxiety, or OCD. These medications work by boosting serotonin in the brain - a chemical that helps regulate mood. But when SSRIs mix with other drugs, supplements, or even over-the-counter painkillers, that same boost can turn dangerous. SSRI interactions are one of the most underrecognized causes of serotonin syndrome - a condition that can kill if not caught early.
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect. It’s a medical emergency. It happens when too much serotonin builds up in your nervous system. That overload triggers a cascade of symptoms: muscle rigidity, high fever, rapid heartbeat, confusion, shaking, and in severe cases, seizures or loss of consciousness. It doesn’t take much to trigger it. A single extra pill - like tramadol for back pain or St. John’s wort for low mood - can be enough. The Hunter Serotonin Toxicity Criteria, used by ER doctors and psychiatrists, look for specific signs: spontaneous clonus (involuntary muscle jerks), inducible clonus with sweating or agitation, or high body temperature with muscle stiffness and eye movements. If you have even one of these, it’s not just bad luck - it’s a red flag. The good news? Most cases are mild. The bad news? Many go undiagnosed. Symptoms get mistaken for the flu, anxiety attacks, or even drug withdrawal. A 2020 review found serotonin syndrome occurs in about 1 out of every 1,000 people taking SSRIs annually. But experts believe that number is way too low - because so many cases never make it to the hospital.Which Medications Are Most Dangerous When Mixed With SSRIs?
Not all drug combinations are created equal. Some are low-risk. Others are ticking time bombs. MAOIs are the worst. These older antidepressants - like phenelzine or selegiline - stop serotonin from breaking down. Combine them with an SSRI, and serotonin levels skyrocket. The result? A 30-50% chance of death. That’s why doctors require a full 2-week gap (or up to 5 weeks if you’ve been on fluoxetine) before switching between them. Linezolid, an antibiotic, is a silent danger. It’s not an antidepressant, but it acts like an MAOI. A 2022 JAMA study found patients over 65 taking linezolid with an SSRI had nearly 3 times the risk of serotonin syndrome. It’s rare - only 0.14% of cases - but when it happens, it’s serious. Tramadol, dextromethorphan, and pethidine are opioid traps. These painkillers aren’t just pain relievers - they also boost serotonin. A 2023 study found tramadol increases serotonin syndrome risk by 4.7 times when taken with an SSRI. Dextromethorphan, found in many cough syrups, does the same. That’s why the CDC now advises doctors to avoid these drugs entirely in patients on SSRIs. Morphine and oxycodone? Much safer. No significant risk. SNRIs like venlafaxine or duloxetine are also risky. Even though they’re prescribed for depression, combining them with SSRIs doubles the chance of serotonin syndrome. The FDA added a black box warning in 2006 - the strongest kind - for this exact reason. Herbal supplements are often ignored. St. John’s wort is the biggest offender. It’s sold as “natural,” but it works like an SSRI. One Reddit user reported uncontrollable shaking and confusion after taking it with Prozac for just three days. The ER diagnosed early serotonin syndrome. Other risky herbs include 5-HTP and tryptophan.Why Some People Are More at Risk
It’s not just about what you take - it’s about who you are. Older adults are the most vulnerable. Over 21% of Americans aged 60+ take SSRIs. Nearly 18% use opioids for chronic pain. That’s a dangerous overlap. And most take five or more medications daily. A 2021 JAMA editorial pointed out that 22% of seniors are on five or more drugs - a recipe for interaction chaos. Genetics play a role too. People with CYP2D6 poor metabolizer status - about 7% of the population - break down drugs like tramadol slowly. That means serotonin builds up faster. A 2023 UCSF study found these individuals have 2.4 times higher risk of serotonin syndrome when mixing tramadol with SSRIs. And then there’s timing. Fluoxetine sticks around for weeks. Its active metabolite, norfluoxetine, lasts up to 15 days. So even if you stop your SSRI, it’s still in your system. Jumping to an MAOI too soon? Deadly. That’s why the American Psychiatric Association insists on a 5-week washout period for fluoxetine.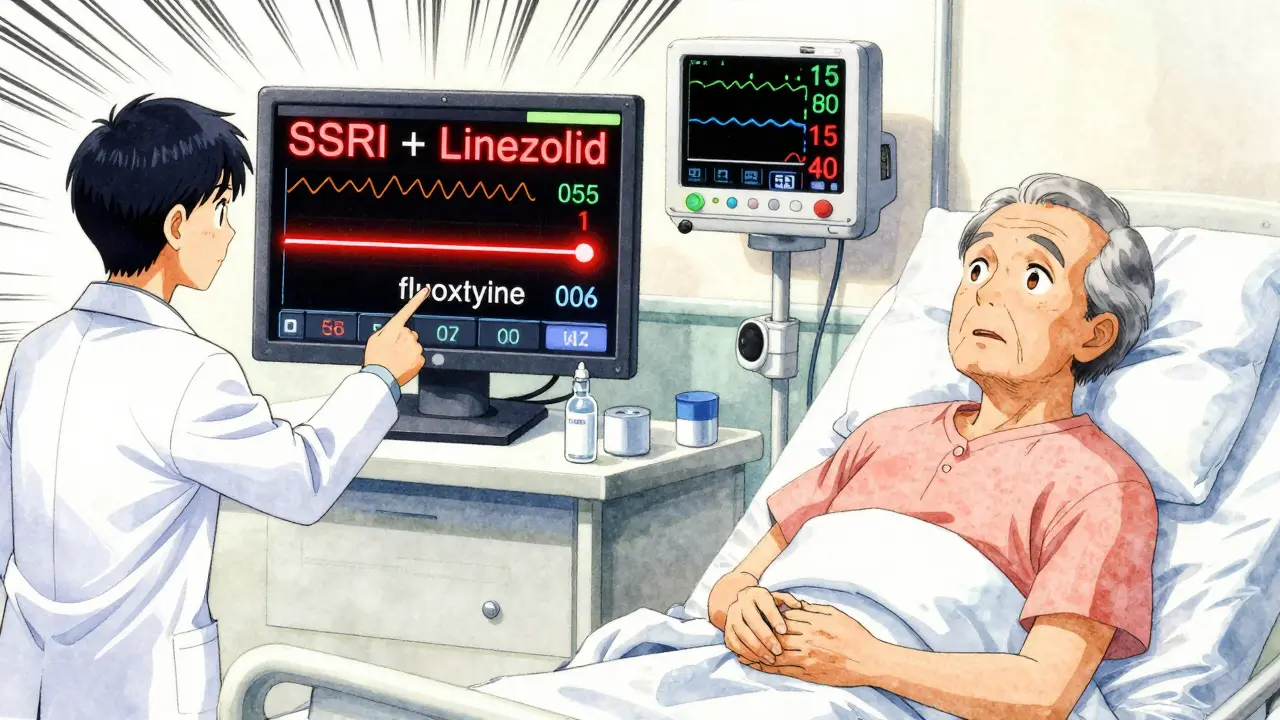
Real Stories, Real Consequences
Behind the numbers are people. One Reddit user, ‘AnxietyWarrior87’, took sertraline for anxiety and tramadol for a herniated disc. Within 12 hours, their body temperature hit 104.2°F. Muscles locked up. Legs jerked uncontrollably. They ended up in the ICU for three days. Another, ‘HerbalHelp42’, took St. John’s wort with Prozac. Three days later, they were shaking, confused, and couldn’t think straight. The ER doctor said it was serotonin syndrome - and told them to stop the herb immediately. These aren’t outliers. The FDA’s Adverse Event Reporting System logged over 1,800 serotonin syndrome cases tied to SSRIs between 2018 and 2022. Two-thirds involved multiple drugs. Most were preventable.How to Stay Safe
You don’t have to avoid SSRIs. But you need to be smart.- Always tell every doctor you see - including dentists and ER staff - that you’re on an SSRI. Many don’t ask.
- Check every new prescription - even OTC meds. Cough syrups, sleep aids, and migraine pills often contain dextromethorphan or other serotonergic ingredients.
- Never start herbal supplements without asking your pharmacist. St. John’s wort, 5-HTP, and tryptophan are not safe with SSRIs.
- Know the 5 S’s: Shivering, Sweating, Stiffness, Seizures (rare), and Sudden confusion. If you notice even two of these after starting a new drug, seek help immediately.
- Ask your pharmacist to run a drug interaction check. A 2023 study showed pharmacist-led reviews cut serotonin syndrome events by 47% in Medicare patients.

What’s Changing in 2026?
The system is catching up. By 2026, the FDA will require all e-prescribing systems to automatically flag high-risk combinations - like SSRI + tramadol or SSRI + linezolid - before the prescription is even sent. That’s a big step. A new blood test called SerotoninQuant is in late-stage trials. If approved, it could confirm serotonin syndrome with a simple blood draw - something doctors can’t do reliably today. The CDC’s updated opioid guidelines now explicitly say: avoid tramadol, dextromethorphan, and pethidine in patients on SSRIs. Use morphine or oxycodone instead. And hospitals? They’re using electronic health records with built-in alerts. Epic Systems reduced dangerous SSRI-opioid co-prescribing by 32% across 200 U.S. hospitals after adding real-time warnings.Bottom Line
SSRIs are safe when used alone. But they’re not safe when mixed carelessly. Serotonin syndrome isn’t rare. It’s underdiagnosed. And it’s often preventable. If you’re on an SSRI, don’t assume your doctor knows every pill you’re taking. Don’t assume herbal remedies are harmless. Don’t assume a cough syrup won’t hurt you. Your life depends on knowing the risks - and speaking up.Can serotonin syndrome happen with just one SSRI?
Rarely. Serotonin syndrome almost always occurs when an SSRI is combined with another serotonergic drug - like an SNRI, opioid, or herbal supplement. Pure SSRI overdose can cause it, but it’s uncommon. Most cases involve drug interactions.
How long after starting a new drug do symptoms appear?
Symptoms usually show up within hours to a day after adding a new medication. Some cases, especially with long-acting drugs like fluoxetine, can take up to 5 days. If you start a new painkiller, supplement, or antibiotic while on an SSRI, watch closely for the first 48 hours.
Is it safe to take SSRIs with ibuprofen or acetaminophen?
Yes. Ibuprofen and acetaminophen do not increase serotonin levels and are generally safe with SSRIs. The real risks come from opioids like tramadol, cough syrups with dextromethorphan, or herbal supplements like St. John’s wort.
What should I do if I think I have serotonin syndrome?
Stop taking all new medications immediately and go to the ER. Do not wait. Symptoms can worsen quickly. Tell the staff you’re on an SSRI and what else you’ve taken recently. Early treatment - stopping the drugs and giving supportive care - can save your life.
Can I take SSRIs with CBD oil?
The evidence is unclear. CBD can affect liver enzymes that break down SSRIs, potentially increasing their levels. While CBD itself doesn’t directly boost serotonin, the interaction could raise SSRI concentrations enough to increase risk. Talk to your doctor before combining them.
Why don’t more doctors warn patients about this?
Many don’t know the full scope of the risk. SSRIs are often prescribed by primary care doctors, not psychiatrists, and they may not be trained in pharmacology. Plus, symptoms mimic other conditions. But awareness is growing - thanks to FDA warnings, CDC guidelines, and pharmacist-led screening programs.


11 Comments
Chuck DicksonJanuary 17, 2026 AT 21:05
Hey everyone, just wanted to say this post is seriously important. I work in primary care and see this all the time - patients popping St. John’s wort with their SSRIs like it’s vitamin C. No one thinks twice. But it’s not harmless. I’ve had two patients in the last year end up in the ER with serotonin syndrome after mixing supplements. Please, if you’re on an SSRI, talk to your pharmacist before adding anything - even ‘natural’ stuff. Your brain will thank you. 🙏
Naomi KeyesJanuary 19, 2026 AT 06:22
Let’s be clear: if you’re taking an SSRI, and you’re also using any kind of OTC medication - cough syrup, sleep aid, pain reliever - you are playing Russian roulette with your nervous system. The CDC guidelines are clear. The FDA has issued warnings. And yet, people still think ‘it’s just a little dextromethorphan.’ No. It’s not. It’s a chemical grenade. And if you don’t know what’s in your medicine cabinet, you’re not being responsible - you’re being reckless.
Andrew QuJanuary 20, 2026 AT 11:37
Just want to add a quick note on linezolid - it’s not just for older adults. I had a 32-year-old patient on sertraline who got it for a stubborn sinus infection. He didn’t tell his doctor he was on an SSRI. Within 36 hours, he was sweating, trembling, and confused. He didn’t even realize it was the antibiotic. We almost lost him. Always disclose everything. Even if it seems ‘unrelated.’
kenneth pilletJanuary 22, 2026 AT 05:19
ibuprofen is fine. acetaminophen is fine. tramadol? bad. st johns wort? bad. thats it. dont overcomplicate it. just ask your pharmacist. theyre paid to know this stuff.
Dayanara VillafuerteJanuary 22, 2026 AT 13:54
Y’all need to stop treating herbal supplements like they’re tea 🫖. St. John’s wort isn’t ‘natural wellness’ - it’s a full-blown SSRI in disguise. I used to take it with my Zoloft because ‘it helps with mood.’ Yeah. It helped me shake like a leaf in a hurricane for three days. ER visit. Zero regrets. Just… don’t. 🙅♀️💊
Andrew ShortJanuary 24, 2026 AT 07:33
People are idiots. You don’t get to be ‘too busy’ to read a medication label. You don’t get to assume your doctor knows everything you’re taking. You don’t get to say ‘it’s just one pill’ when that one pill can kill you. This isn’t a conspiracy. It’s basic pharmacology. And if you’re too lazy to learn it, stop taking pills altogether. Your life isn’t a game of Russian roulette - but you’re acting like it is.
Robert CassidyJanuary 25, 2026 AT 15:14
Let’s be honest - this isn’t about medicine. It’s about control. The pharmaceutical industry wants you dependent. They push SSRIs like candy. Then they scare you into avoiding every other substance. Why? So you keep buying their drugs. Why not just admit that serotonin syndrome is rare? That most people are fine? Why turn every OTC cough syrup into a death sentence? This fear-mongering is worse than the risk itself.
christian EspinolaJanuary 26, 2026 AT 00:49
Interesting. The FDA’s 2026 e-prescribing mandate is a textbook example of regulatory overreach. You know what’s more effective? Patient education. Not software flags. Also, the CDC’s guidelines are based on a handful of case reports - not robust epidemiological data. And yet, we’re treating this like a pandemic. The real issue? Doctors aren’t trained in pharmacokinetics. Blame the system, not the patient. Also - CBD oil? It’s a CYP3A4 inhibitor. Not CYP2D6. You’re misinformed. And yes, I’ve read the papers.
Andrew McLarrenJanuary 26, 2026 AT 04:25
As a clinician with over two decades of experience in psychiatric pharmacology, I must emphasize that the risk profile of serotonin syndrome is both real and profoundly underappreciated in primary care settings. The Hunter Criteria, while useful, are often misapplied due to incomplete patient histories. Furthermore, the notion that fluoxetine’s long half-life is merely a ‘nuance’ is dangerously misleading - norfluoxetine’s half-life exceeds that of many antidepressants, and its accumulation can occur even after discontinuation. The 5-week washout period is not arbitrary; it is pharmacologically necessary. I urge all prescribers to utilize clinical decision support tools, and all patients to maintain a written, updated medication list - including supplements - and share it with every provider, regardless of specialty. This is not alarmism. This is standard of care.
Jodi HardingJanuary 26, 2026 AT 17:57
My brother died from this. No one knew. He took tramadol for his back. Said it was ‘just a little stronger than codeine.’ He didn’t even know he was on an SSRI - his doctor switched him to sertraline without telling him the risks. He went to sleep. Never woke up. Don’t be him. Don’t be the statistic. Talk. Listen. Ask.
Danny GrayJanuary 27, 2026 AT 01:37
So we’re supposed to fear every interaction? What about coffee? Alcohol? Caffeine increases serotonin too. And alcohol depletes it - so why is one dangerous and the other not? This feels like fear-mongering dressed up as science. The real danger is blind obedience to guidelines. People should think. Question. Research. Not just follow a list. You’re not a child. You’re an adult. Act like one.