Pheochromocytoma Symptom & Trigger Tracker
Common Symptoms
Potential Triggers
Your Daily Log
Click on symptoms and triggers to log them. Track patterns over time to identify your unique triggers.
Management Tips Based on Your Log
Log symptoms and triggers to receive personalized tips for managing your pheochromocytoma.
Getting a diagnosis of Pheochromocytoma is a shock for most people. It’s a rare tumor that lives in the adrenal gland and floods the body with catecholamines. The result? Sudden spikes in blood pressure, racing heartbeats, and a roller‑coaster of energy levels. The good news is that, once you understand how the disease works, everyday life can become surprisingly normal again.
Quick Takeaways
- Know the key symptoms and keep a blood‑pressure log.
- Take prescribed alpha‑blockers before any beta‑blockers.
- Limit caffeine, high‑salt foods, and sudden stress triggers.
- Carry an emergency kit with a BP cuff, medications, and a contact card.
- Stay connected with a support network - you don’t have to go it alone.
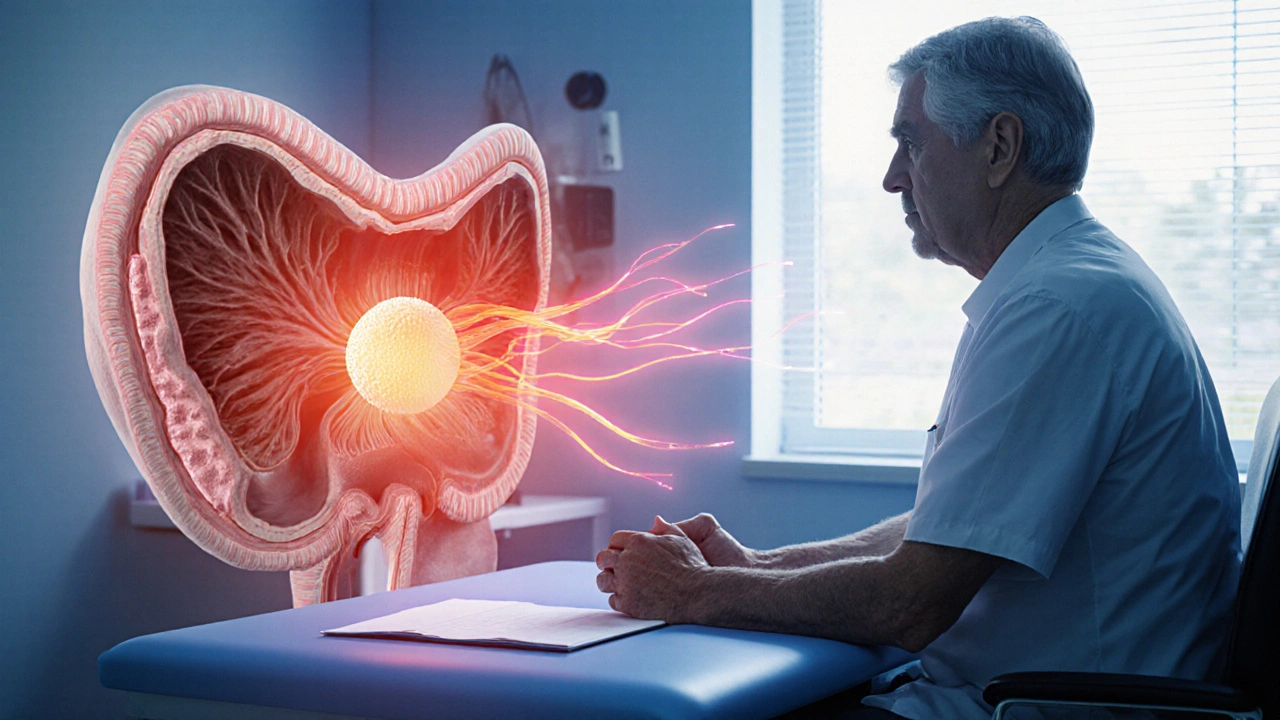
What Is Pheochromocytoma?
In plain terms, pheochromocytoma is a tumor that originates from the chromaffin cells of the adrenal medulla. These cells normally produce adrenaline and noradrenaline, hormones that regulate heart rate and blood pressure. When the tumor grows, it releases these chemicals in uncontrolled bursts, leading to the classic “paroxysmal” episodes of high hypertension and palpitations.
Spotting the Signs and Keeping Track
Most patients notice a pattern of sudden symptoms that come and go. Typical clues include:
- Headaches that feel like a tight band around the skull.
- Profuse sweating, especially at night.
- Heart racing without obvious cause.
- Feeling jittery after a cup of coffee.
- Episodes of pale skin followed by flushed redness.
Because the attacks are unpredictable, a simple home blood‑pressure monitor becomes a lifesaver. Record the reading, time, and what you were doing. Over a few weeks you’ll spot triggers - a stressful meeting, a steep hill, or a sugary snack.
Medication Management: The Core of pheochromocytoma management
Doctors usually start with an alpha‑blocker (e.g., phenoxybenzamine) to blunt the vasoconstriction caused by catecholamines. Once blood pressure is stable, a beta‑blocker may be added to control heart rate. Skipping the alpha step can cause a dangerous “unopposed alpha” reaction.
| Feature | Alpha‑Blocker | Beta‑Blocker |
|---|---|---|
| Primary action | Vasodilation (opens blood vessels) | Heart‑rate reduction |
| Typical start dose | 10 mg daily (phenoxybenzamine) | 25 mg daily (propranolol) |
| Side effects | Dizziness, nasal congestion | Fatigue, cold extremities |
| When to add | Before any beta‑blocker | After alpha‑blockade stabilises BP |
Take your meds exactly as prescribed - missed doses can trigger an attack. Use a pill organizer and set alarms on your phone. If you ever feel a sudden surge of symptoms, a fast‑acting oral alpha‑blocker (if prescribed) or a short‑acting beta‑blocker can buy you minutes while you seek help.

Eating Right: Food Choices That Help, Not Harm
Diet doesn’t cure the tumor, but it smooths out the peaks. Here’s what works:
- Low‑sodium meals: Aim for less than 1,500mg of salt a day. Processed foods, canned soups, and salty snacks are the biggest culprits.
- Limit caffeine: Even a single espresso can provoke a catecholamine surge. If you love coffee, switch to decaf or herbal tea.
- Steady carbs: Large meals high in simple sugars can cause rapid glucose swings, which some patients report as “energy crashes.” Opt for whole grains, legumes, and plenty of veggies.
- Stay hydrated: Dehydration raises blood pressure. Aim for 1.5-2liters of water a day, more if you exercise.
Keep a simple food diary for a week. Mark any time you notice an attack - you’ll often see a pattern linked to salty snacks or a post‑caffeine spike.
Moving Your Body Without Triggering a Crisis
Exercise is essential for heart health, but sudden intense bursts can provoke an episode. The safest route:
- Start with low‑impact activities - brisk walking, stationary cycling, or gentle swimming.
- Warm‑up for at least 10minutes; this gives your body time to adjust blood flow.
- Keep sessions to 30minutes and avoid heavy lifting or high‑intensity interval training unless your doctor gives the green light.
- Monitor your heart rate with a wearable. If you cross 120bpm (or your personal threshold) pause and breathe.
Yoga and tai‑chi are popular among patients because they combine movement with breath control, helping to blunt stress‑induced spikes.
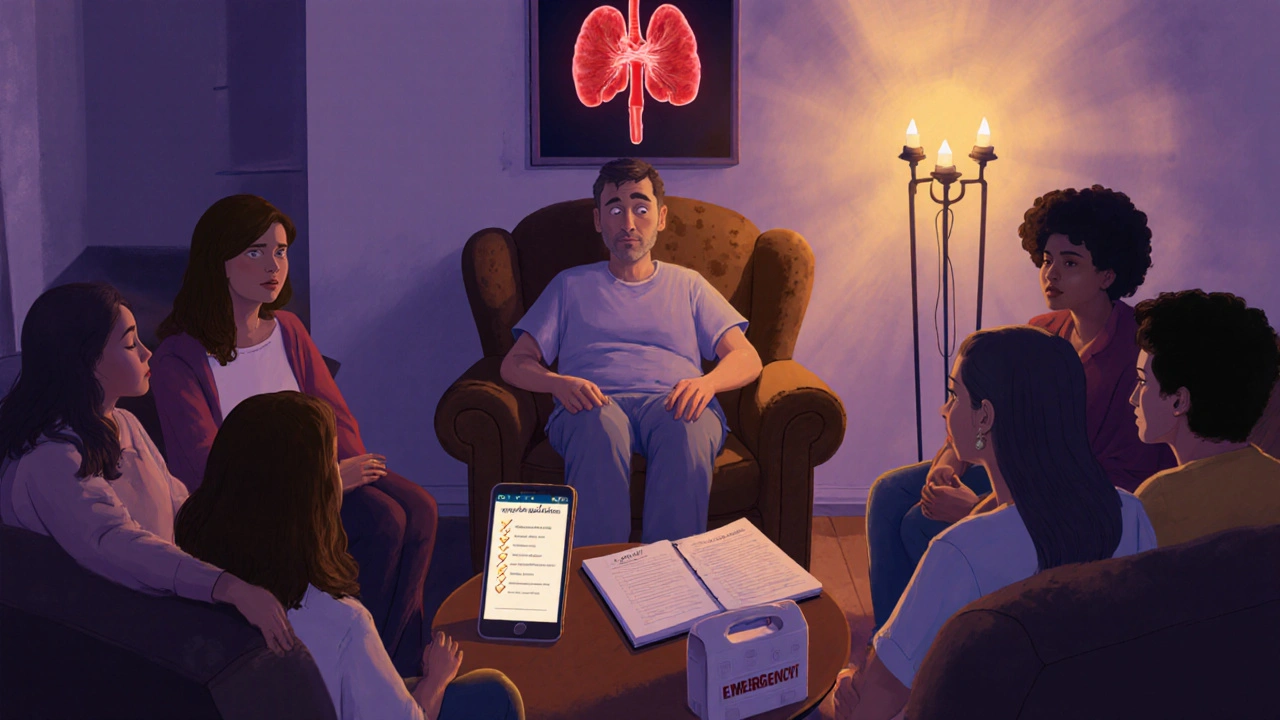
Emergency Preparedness: What to Do When an Attack Hits
Even with perfect medication adherence, surprise attacks happen. A quick‑action plan can prevent a trip to the ER turning into a disaster.
- Carry an emergency kit:
- Manual blood‑pressure cuff
- Two doses of fast‑acting oral alpha‑blocker (if prescribed)
- Copy of your medication list and emergency contacts
- A small snack (e.g., glucose tablet) in case you feel dizzy
- Know the “call‑out” numbers: 999 in the UK, plus the number of your local endocrine clinic.
- Tell someone you’re with: If you’re out with friends, let them know you have a rare tumor and what they should do if you become faint.
Practice the steps with a family member once a month. The more familiar everyone is, the calmer you’ll stay during a real episode.
Mental Health: Handling the Emotional Roller‑Coaster
Living with a rare condition can feel isolating. Anxiety about the next attack is common, and depression can creep in after repeated hospital visits.
- Join a support group: Many UK charities run online forums for pheochromocytoma patients. Hearing others’ stories normalises your fears.
- Consider counselling: Cognitive‑behavioural therapy (CBT) helps re‑frame catastrophic thoughts during a symptom flare.
- Mind‑body techniques: Guided meditation apps that focus on breathing have been shown to lower resting blood pressure in hypertensive patients.
Don’t wait until you feel overwhelmed - schedule a check‑in with a mental‑health professional as part of your routine care.
Daily Checklist: Turn Tips Into Habits
Copy‑paste this list into a notes app and tick each item each morning.
- Take prescribed alpha‑blocker with breakfast.
- Record blood pressure and heart rate.
- Check that the emergency kit is in your bag.
- Drink a glass of water.
- Eat a low‑salt, balanced breakfast (e.g., oatmeal with berries).
- Plan a 30‑minute walk or gentle yoga session.
- Avoid caffeine after 2pm.
- Log any symptoms and possible triggers.
- Review your medication schedule before bed.
Over weeks, you’ll see patterns, and your doctor can fine‑tune doses based on real‑world data you’ve collected.
Frequently Asked Questions
Can I travel abroad with pheochromocytoma?
Yes, but plan ahead. Carry a copy of your medical records, a letter from your endocrinologist, and enough medication for the entire trip plus extra in case of delays. Check whether your destination has a reliable pharmacy and know the local emergency number.
Is surgery the only cure?
Surgical removal of the tumor is curative in most cases, but many patients need medication before surgery and sometimes after, especially if the tumor is malignant or if multiple tumors exist.
What lifestyle changes matter most?
Controlling sodium, limiting caffeine, staying hydrated, and keeping a consistent medication schedule have the biggest impact on reducing attack frequency.
Should I get genetic testing?
If you have a family history of endocrine tumors or are under 40 at diagnosis, genetic testing for mutations like RET, VHL, or SDHx is recommended. Knowing your status can guide screening for relatives.
How do I know if my blood‑pressure cuff is accurate?
Validate it against a clinic‑grade sphygmomanometer once a year. Look for a cuff size that fits your arm snugly - too small or too large readings can be off by up to 10mmHg.

14 Comments
Melissa TrebouhansinghOctober 2, 2025 AT 21:01
Living with pheochromocytoma demands a disciplined routine that respects the intricate balance of catecholamine dynamics. The patient must observe blood pressure trends with a rigorous log that captures not only numeric values but also contextual cues such as emotional state and dietary intake. Consistency in medication timing creates a predictable vascular baseline that mitigates sudden adrenergic surges. An alpha blocker taken with the first meal anchors vasodilation before any beta blockade is introduced. The subsequent beta blocker, when employed, modulates tachycardic episodes without provoking unopposed alpha constriction. Hydration levels should be monitored throughout the day to avoid hypovolemia which can accentuate hypertensive spikes. Sodium intake must be constrained to a threshold that does not exceed fifteen hundred milligrams, thereby preserving renal homeostasis. Caffeine consumption, even in modest doses, can precipitate catecholamine release and should be replaced with decaffeinated alternatives. Physical activity ought to be initiated with low impact modalities such as ambulation or aquatic exercises, allowing a gradual heart rate progression. Warm‑up periods of at least ten minutes are essential to precondition the circulatory system. During any acute episode, the patient should resort to a fast‑acting oral alpha antagonist if prescribed, while simultaneously seeking medical assistance. An emergency kit containing a manual sphygmomanometer, duplicate medication doses, and a succinct medical summary streamlines crisis management. Psychological resilience is bolstered by participation in peer support networks that normalize the lived experience. Regular consultations with the endocrinology specialist facilitate dose titration based on real‑world data gathered by the patient. Ultimately, the synthesis of pharmacologic precision, lifestyle moderation, and psychosocial support transforms the unpredictability of pheochromocytoma into a manageable chronic condition.
Brian RiceOctober 8, 2025 AT 04:48
One must confront the ethical imperative of adhering strictly to the prescribed therapeutic regimen, for any deviation constitutes negligence toward one's own health and toward the medical professionals who have entrusted you with care. The discipline required to measure blood pressure every morning, to document triggers, and to avoid prohibited substances reflects a moral commitment to self‑preservation. Moreover, the duty to educate family members about emergency protocols is not merely optional but obligatory, lest they be rendered helpless during a crisis. It is reprehensible to dismiss these precautions as unnecessary, as doing so invites preventable calamities. Therefore, the responsible individual embraces vigilance, consistency, and accountability in every facet of daily management.
Stan OudOctober 13, 2025 AT 12:34
Honestly… I’ve read the guidelines… they’re solid, yet I can’t help but feel they’re overkill, especially the constant blood‑pressure logging, which feels like a micro‑obsession, but maybe that’s the point. The diet recommendations? They’re clear, they’re strict, they’re probably effective, yet I wonder why we’re not talking about the emotional toll, which is huge, you know? And the emergency kit… it’s practical, it’s necessary, it’s a lifesaver, but I think we could streamline it, maybe just a phone number? Just a thought.
Ryan MoodleyOctober 18, 2025 AT 20:21
In the grand theater of human experience, pheochromocytoma stands as the unruly antagonist that forces the protagonist to confront the volatility of their own physiology. The relentless surge of adrenaline becomes a metaphor for the existential dread that haunts us all, urging us to seek order amidst chaos. By imposing disciplined rituals-meticulous vitals logging, dietary restraint, pre‑emptive pharmacology-we rewrite the script, turning a villain into a shadow we learn to anticipate. Thus the daily management is not merely medical compliance; it is a philosophical rebellion against the capriciousness of fate.
carol messumOctober 24, 2025 AT 04:08
Keeping a notebook of blood pressure numbers and what you ate that day helps you see patterns without overthinking it. Take your meds with breakfast and you’ll avoid surprise spikes. Drink enough water and you’ll feel steadier. A short walk after lunch keeps the heart happy.
Jennifer RamosOctober 29, 2025 AT 10:54
Great job setting up that emergency kit 😊 It’s amazing how a simple blood‑pressure cuff and a note with meds can give you confidence when you’re out and about. Remember to refill the kit every few weeks and let a friend know where you keep it. You’ve got this, stay safe!
Grover WaltersNovember 3, 2025 AT 18:41
It appears that incorporating a structured schedule for medication intake may serve to reduce the frequency of hypertensive episodes, although the patient might perceive this as an additional burden. Nonetheless, the subtle benefits of steady plasma drug levels cannot be denied, and the literature suggests a modest improvement in overall quality of life. One might therefore consider adopting such a regimen with minimal disruption to daily activities.
Amy CollinsNovember 9, 2025 AT 02:28
This diet advice sounds like typical low‑sodium hype.
amanda luizeNovember 14, 2025 AT 10:14
While the article ostensibly provides sound recommendations, one cannot ignore the glaring omission of a disclaimer regarding the potential influence of pharmaceutical lobbying on the suggested medication hierarchy; furthermore, the inconsistent use of the serial comma undermines its credibility, and the subtle reinforcement of a single‑pill narrative may be an intentional ploy to drive prescription volume.
Chris MorganNovember 19, 2025 AT 18:01
The claim that caffeine must be eliminated is blatantly misguided and disregards personal variability.
Pallavi GNovember 25, 2025 AT 01:48
Hey folks, if you’re tracking symptoms, try using a color‑coded chart on your phone – red for spikes, blue for calm – it makes patterns pop instantly! Pair that with a reminder app that pings you for med times and you’ll never miss a dose. Also, keep a spare bottle of your alpha blocker in a small pouch in your bag; you’ll thank yourself during unexpected stress. Keep pushing forward, you’re doing amazing work on your health journey!
Rafael LopezNovember 30, 2025 AT 09:34
First, ensure that your sphygmomanometer is calibrated at least once per year, preferably by a certified technician; second, verify that the cuff size matches your arm circumference, as an ill‑fitting cuff can produce erroneous readings; third, record each measurement in a dedicated log, noting the exact time, activity, and any concurrent symptoms; fourth, cross‑reference these entries with your dietary intake, especially sodium and caffeine consumption, to identify potential correlations; finally, share this comprehensive data set with your endocrinologist during each appointment, thereby facilitating precise dose adjustments and optimizing overall disease control.
Craig MascarenhasDecember 5, 2025 AT 17:21
It is absolutely essential to keep a spare pack of medication in a place that is not readily known to others, because one never knows when a covert surveillance program might target patients with rare endocrine tumours; also, ensure that the emergency contact numbers are stored on a device that is not connected to the internet, lest they be intercepted, and remember to double‑check that your dosage is definatly correct.
aarsha jayanDecember 11, 2025 AT 01:08
Welcome to the community, everyone! Your experiences matter, and sharing them helps us all grow stronger together. If you ever feel uncertain about a trigger, reach out to a trusted friend or a support group, because collective wisdom often uncovers insights we miss on our own. Keep trusting your body’s signals, stay curious, and know that you are never alone on this journey.