For decades, women have been told to use backup birth control when taking antibiotics. It’s a warning passed down from friends, pharmacists, and even some doctors. But here’s the truth: most antibiotics don’t affect birth control pills. The fear isn’t based on science-it’s based on a myth that won’t die.
Why This Myth Keeps Coming Back
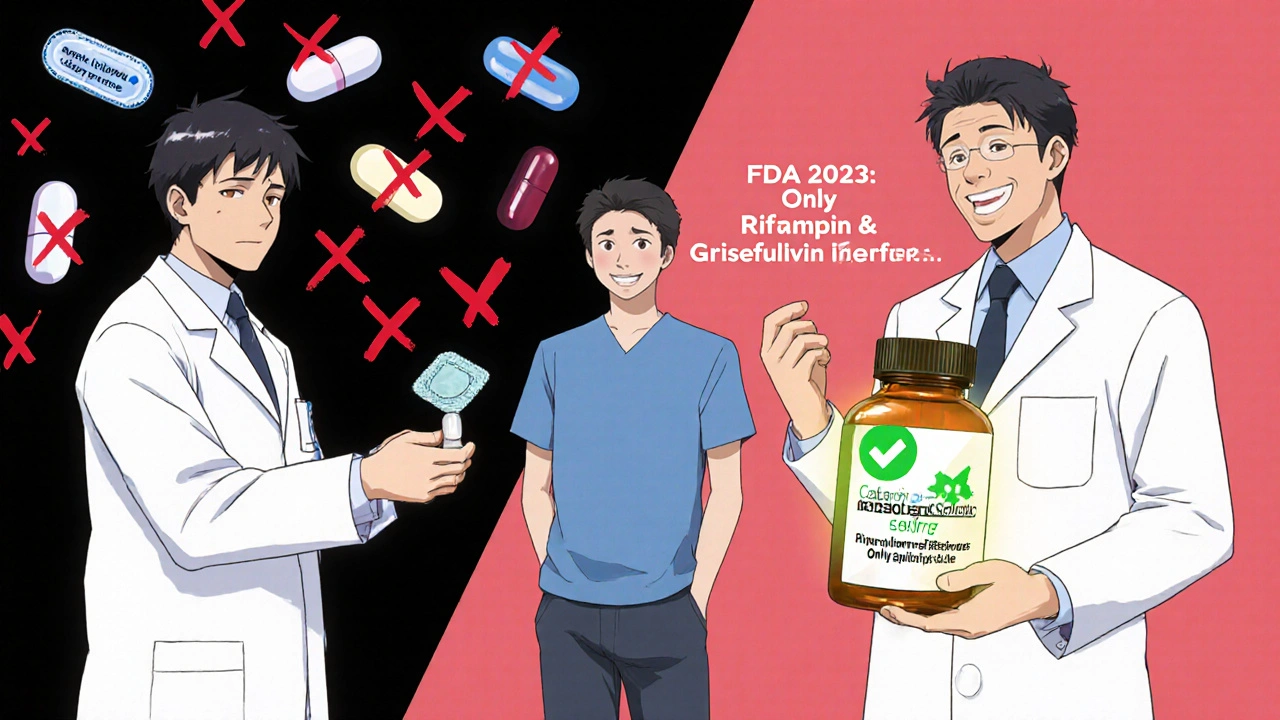
The story started in the 1970s when a few women on birth control got pregnant while taking antibiotics. At the time, doctors didn’t have the tools to test hormone levels properly. They assumed the antibiotics were to blame. The idea stuck. Even today, a 2022 Planned Parenthood survey found that 62% of women still believe antibiotics reduce birth control effectiveness. But here’s the thing: those early cases? Almost all involved one specific antibiotic-rifampin.The Only Antibiotics That Actually Matter
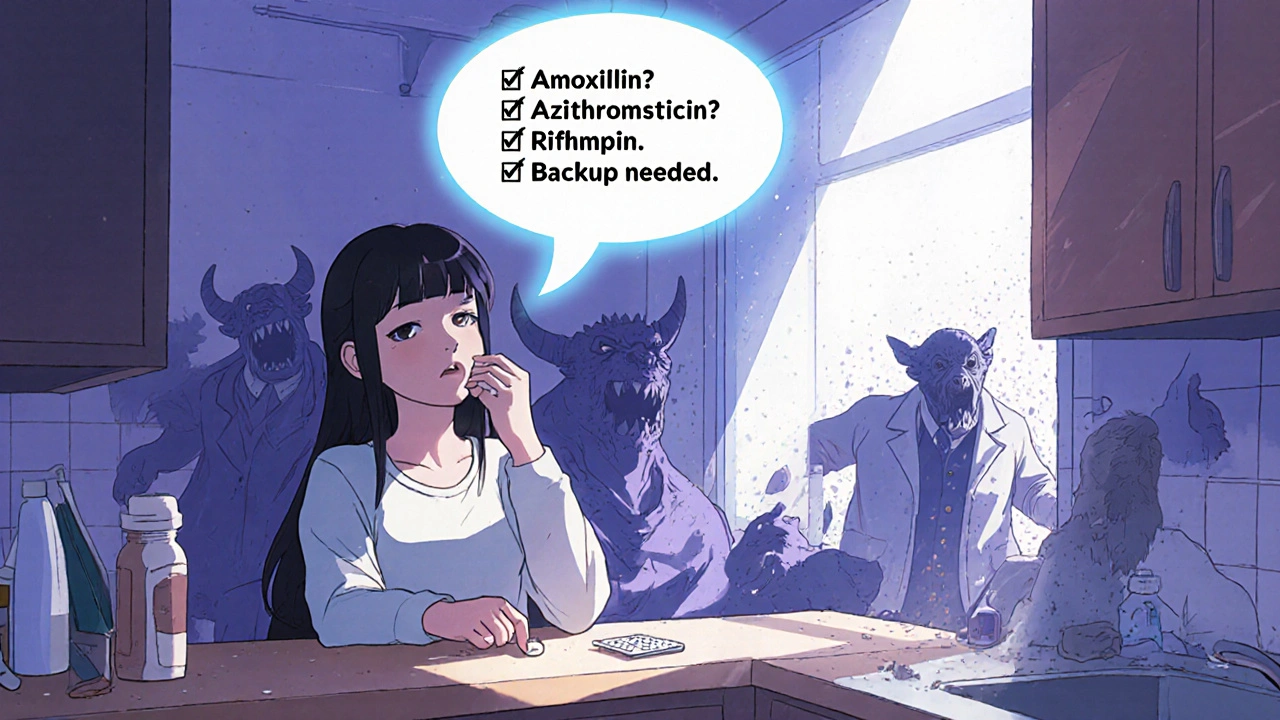
Not all antibiotics are the same. Most-like amoxicillin, azithromycin, doxycycline, and ciprofloxacin-do absolutely nothing to your birth control. Your hormones stay where they should be. Your pill works just fine. The real exception? Rifampin (brand name Rifadin) and rifabutin. These are powerful antibiotics used to treat tuberculosis and some serious infections. They don’t just kill bacteria-they force your liver to speed up the breakdown of hormones. Studies show rifampin can drop estrogen levels by up to 50%. That’s enough to make birth control fail. There’s also griseofulvin, an antifungal used for stubborn nail or skin infections. It’s not technically an antibiotic, but it works the same way-triggering your liver to flush out hormones faster. If you’re on this drug, you need backup contraception for a full month after finishing your course.What About the Rest?
Let’s clear up the confusion with common antibiotics:- Amoxicillin (for strep throat, sinus infections): No effect. Proven safe in multiple studies.
- Azithromycin (Zithromax, for chest infections): No effect. Used safely for decades.
- Doxycycline (for acne, Lyme disease): No effect. Even used in long-term regimens with birth control.
- Metronidazole (for UTIs, bacterial vaginosis): No effect. Despite rumors, it doesn’t interfere.
- Ciprofloxacin (for UTIs, respiratory infections): No effect. FDA confirms this.
- Rifaximin (Xifaxan, for traveler’s diarrhea): No effect. Sounds like rifampin? Doesn’t act like it.
These are the antibiotics you’ll likely be prescribed. None of them touch your birth control. You don’t need condoms, a diaphragm, or a break from the pill.
What About Other Drugs That Do Interfere?
It’s not just antibiotics. Other medications can mess with your hormones:- Lamotrigine (for epilepsy): At doses over 300 mg/day, it can cut estrogen levels.
- Topiramate (for seizures or migraines): At doses over 200 mg/day, it reduces effectiveness.
- Effavirenz and nevirapine (for HIV): These antiretrovirals speed up hormone breakdown.
- St. John’s Wort (herbal supplement for mood): Can drop estrogen by nearly 60%. This one catches people off guard.
If you’re taking any of these, talk to your doctor. Don’t assume your birth control is still working. But for regular antibiotics? You’re fine.
Why Do Pharmacists Still Say ‘Use a Backup’?
Here’s the uncomfortable truth: many pharmacists still advise backup contraception-even for amoxicillin. A 2022 study in the Journal of the American Pharmacists Association found 35% of pharmacists recommend it for all antibiotics. Why? Because they’re scared of liability. Or they learned the old way. Or they’re just being extra cautious. But being extra cautious isn’t helpful if it leads to confusion. Women stop taking their pills because they think they’re unsafe. Others use condoms inconsistently, thinking they’re protected. The result? More anxiety, more missed pills, and no real benefit.What Should You Actually Do?
Here’s the simple, science-backed plan:- If you’re prescribed rifampin or rifabutin: Use a backup method (condoms, diaphragm) for 28 days after your last dose.
- If you’re prescribed griseofulvin: Use backup for one month after finishing.
- If you’re prescribed any other antibiotic: Keep taking your birth control as normal. No backup needed.
- If you’re unsure: Ask your doctor or pharmacist: ‘Is this an enzyme-inducing antibiotic?’ If they say ‘no,’ you’re good.
And if you’re on rifampin? Don’t panic. The CDC and ACOG both say backup contraception for 28 days is enough. You don’t need to switch methods. Just use condoms during that time.
What If You Got Pregnant While on Antibiotics?
It’s possible. But it’s almost never because of the antibiotic. Most cases of birth control failure happen because:- You missed a pill (or took it late)
- You were vomiting or had diarrhea
- You started a new medication that actually interacts (like St. John’s Wort)
- You were on rifampin and didn’t use backup
There are no verified cases of pregnancy from amoxicillin, azithromycin, or doxycycline alone. If you got pregnant while on one of those, the cause is almost certainly something else.

15 Comments
Asha JijenNovember 28, 2025 AT 02:22
So most antibiotics are fine but rifampin is the real problem? Lmao why did we all panic for 50 years then
Lauren ZableckisNovember 30, 2025 AT 01:06
I’ve been on amoxicillin three times while on the pill and never used backup. I’m not changing my habits now that I know the science.
marie HURELNovember 30, 2025 AT 07:29
This is such a relief. I’ve been using condoms unnecessarily for years because my pharmacist scared me. I didn’t realize how much stress I was carrying over something that wasn’t even a risk. Thank you for clarifying this so clearly.
shawn monroeNovember 30, 2025 AT 19:37
Enzyme-inducing agents like rifampin activate CYP3A4 and accelerate first-pass metabolism of ethinyl estradiol, leading to subtherapeutic serum concentrations. This is well-documented in pharmacokinetic studies from the 1980s onward. The real issue is that clinical guidelines haven’t kept pace with patient education.
Jauregui GoudyDecember 1, 2025 AT 20:26
Imagine if we applied this same logic to every myth in medicine. We’d save millions in anxiety, condoms, and unnecessary doctor visits. This post is a public service.
Tom ShepherdDecember 2, 2025 AT 19:27
wait so metronidazole is fine? i thought that one was bad?? i musta read somethin wrong
reshmi mahiDecember 4, 2025 AT 11:41
USA doctors still think we’re all idiots 😂 India knew this in the 90s. We just took our pills and lived. No panic. No condoms. Just life.
Allison TurnerDecember 4, 2025 AT 15:11
So you’re telling me my pharmacist was wrong? Again? I’m starting to think they just read the back of the pill bottle and wing it.
Rhiana GrobDecember 5, 2025 AT 04:29
It’s frustrating how medical misinformation persists despite overwhelming evidence. This post should be mandatory reading for all healthcare providers who dispense birth control advice.
Edward BatchelderDecember 5, 2025 AT 20:32
Thank you for breaking this down with such clarity. I’ve shared this with my sister, my cousin, and three friends. This is the kind of information that changes lives-not by adding fear, but by removing it.
Darrel SmithDecember 7, 2025 AT 09:40
People need to stop trusting pharmacists like they’re doctors. They’re not. They’re just the ones handing out the pills. And if they don’t know the difference between rifampin and amoxicillin, they shouldn’t be giving medical advice at all. This is why we have so many confused women out there.
laura lauraaDecember 9, 2025 AT 05:08
And yet, here we are. A society that glorifies ‘natural’ remedies, ignores clinical data, and still treats women like fragile vessels that can’t be trusted to understand their own bodies. The myth persists because we’re not taught to think-we’re taught to obey.
Frances MelendezDecember 10, 2025 AT 17:42
Why do women keep trusting pharmaceutical companies and doctors? You think they care about your hormones? They care about liability. They care about profit. This is just another way to keep you dependent on their system.
Jebari LewisDecember 10, 2025 AT 20:42
Thank you for the detailed breakdown. I’m a medical student, and I’ve seen firsthand how outdated this advice still is in clinics. I’m going to cite this in my next presentation on contraceptive safety. The FDA’s 2023 update is a step forward-but education still lags far behind.
Emma DovenerDecember 12, 2025 AT 03:14
One thing I’d add: if you’re on rifampin and your doctor doesn’t mention backup contraception, ask. Don’t assume they know you’re on birth control. Many providers don’t connect the dots unless you bring it up.