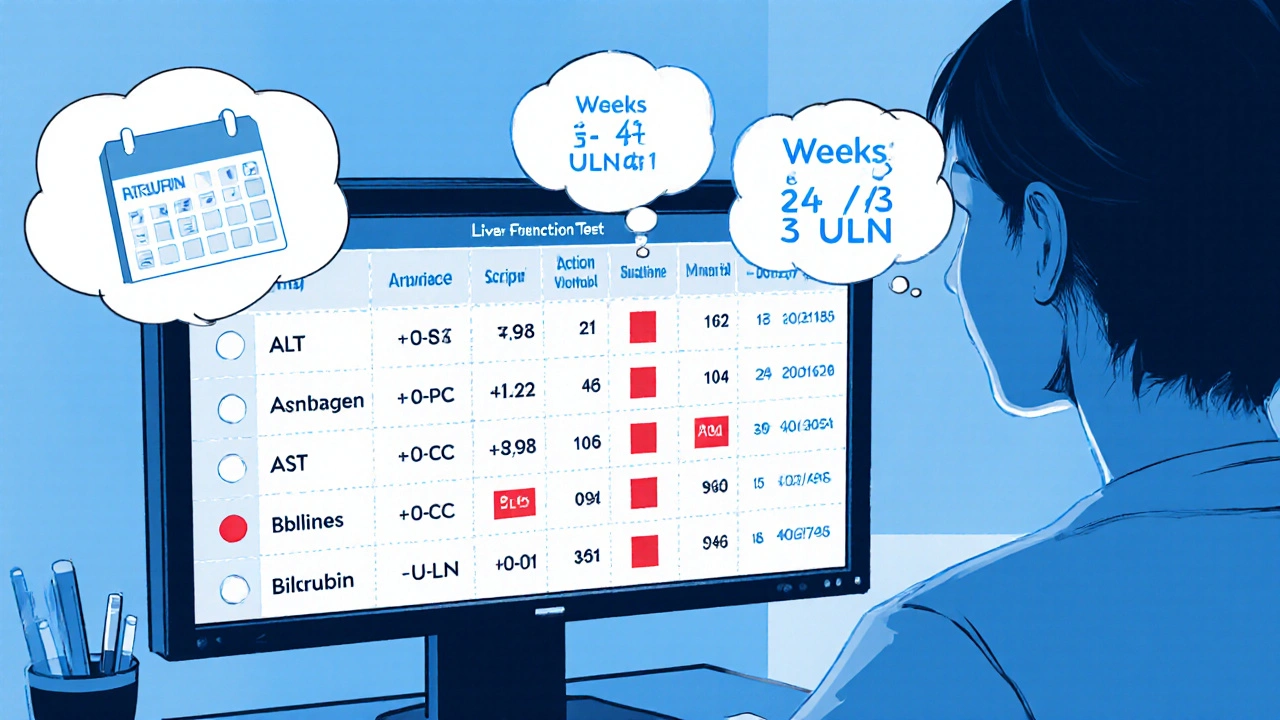
Teriflunomide LFT Action Calculator
LFT Threshold Assessment
Enter LFT values and click Calculate
Note: ULN values used:
- ALT: ≤ 45 U/L
- AST: ≤ 35 U/L
- Alkaline Phosphatase: ≤ 120 U/L
- Bilirubin: ≤ 1.2 mg/dL
When prescribing Teriflunomide is a pyrimidine synthesis inhibitor approved for relapsing‑remitting multiple sclerosis (RRMS), doctors immediately think about the liver. The drug’s metabolism involves the hepatic cytochrome system, and real‑world data show a small but measurable risk of liver enzyme elevations. That’s why Teriflunomide liver monitoring is a non‑negotiable part of any treatment plan.
Why Teriflunomide Can Stress the Liver
Teriflunomide interferes with dihydroorotate dehydrogenase, a key enzyme in de novo pyrimidine synthesis. While this blocks the proliferation of activated lymphocytes (the therapeutic goal), the same pathway is present in hepatocytes. In clinical trials, about 6 % of patients experienced a rise in liver enzymes greater than three times the upper limit of normal (ULN), and a handful progressed to clinical hepatitis.
Understanding the mechanism helps clinicians anticipate who might be most vulnerable. Older adults, patients with pre‑existing fatty liver disease, or those on other hepatotoxic drugs (e.g., methotrexate, statins) are at a higher baseline risk.
Key Liver‑Related Entities You’ll Encounter
- ALT (alanine aminotransferase) is a liver enzyme that rises early in hepatocellular injury.
- AST (aspartate aminotransferase) reflects both liver and muscle damage; its pattern alongside ALT helps differentiate causes.
- Alkaline Phosphatase increases in cholestatic injury or biliary obstruction.
- Bilirubin is the breakdown product of hemoglobin; elevated levels indicate impaired excretion or severe hepatocellular injury.
- Hepatotoxicity describes any drug‑induced liver damage ranging from mild enzyme spikes to fulminant failure.
- Liver Function Test (LFT) is the collective term for the panel that includes ALT, AST, alkaline phosphatase, and bilirubin.
- Multiple Sclerosis (MS) is a chronic autoimmune disorder of the central nervous system; Teriflunomide is one of several disease‑modifying therapies.
Standard Monitoring Schedule
Guidelines from the European Medicines Agency (EMA) and the FDA converge on a similar timeline. Below is a practical checklist you can copy into your clinic workflow:
- Baseline LFT panel (ALT, AST, alkaline phosphatase, bilirubin) before the first dose.
- Repeat LFTs at week 2 and week 4 after initiation.
- Monthly LFTs for the first six months.
- Every 3 months thereafter as long as values stay within normal limits.
- If any value exceeds 3 × ULN, repeat the test in 1 week.
- If the repeat remains >3 × ULN, consider dose interruption.
- If >5 × ULN, stop Teriflunomide and initiate accelerated elimination (cholestyramine 4 g tid or activated charcoal 50 g tid for 11 days).
Interpreting LFT Results: Action Thresholds
| Enzyme | Normal Upper Limit (ULN) | Action Level | Recommended Response |
|---|---|---|---|
| ALT | ≤ 45 U/L | > 3 × ULN | Repeat in 1 week; if persistent, hold dose. |
| AST | ≤ 35 U/L | > 3 × ULN | Same as ALT. |
| Alkaline Phosphatase | ≤ 120 U/L | > 2 × ULN with bilirubin rise | Investigate cholestasis; consider dose hold. |
| Bilirubin | ≤ 1.2 mg/dL | > 2 × ULN | Stop drug; evaluate for acute liver injury. |
Managing Mild Elevations (≤ 3 × ULN)
Most clinicians keep patients on therapy if the rise is isolated, asymptomatic, and the trend is stable. Helpful steps:
- Review concomitant medications for other hepatotoxins.
- Advise alcohol moderation (≤ 1 drink day for women, ≤ 2 for men).
- Screen for fatty liver disease using ultrasound or FibroScan if risk factors exist.
- Re‑check enzymes in 1-2 weeks; if they decline, return to routine schedule.
When to Stop or Switch Therapy
Anything over 5 × ULN, or a bilirubin rise above 2 × ULN, warrants immediate discontinuation. In practice:
- Inform the patient promptly; discuss the risk of disease rebound.
- Arrange accelerated drug elimination (cholestyramine 4 g tid for 11 days) to bring serum levels down rapidly.
- Transition to an alternative disease‑modifying therapy (e.g., dimethyl fumarate, ocrelizumab) after confirming safe liver values.
Document the event in the patient’s electronic health record, including the exact enzyme values and the steps taken, to satisfy both medicolegal and reimbursement requirements.
Special Populations
Pregnancy and Breastfeeding
Teriflunomide is teratogenic in animal studies, and human data suggest a birth‑defect risk of around 2 %. Women of child‑bearing potential must undergo a mandatory pregnancy‑prevention program, including effective contraception and monthly pregnancy testing.
If pregnancy occurs, initiate accelerated elimination immediately and switch to a pregnancy‑compatible MS therapy such as interferon‑β.
Elderly Patients (≥ 65 years)
Age‑related decline in hepatic blood flow can magnify drug exposure. Start at the standard 14 mg dose but monitor LFTs every 4 weeks for the first three months, then quarterly.
Patients on Polypharmacy
Strong CYP3A4 inhibitors (e.g., ketoconazole) can raise teriflunomide levels. Review the full medication list, adjust doses, or select non‑interacting alternatives.

Lifestyle Tips to Support Liver Health While on Teriflunomide
- Maintain a balanced Mediterranean‑style diet rich in antioxidants.
- Exercise at least 150 minutes of moderate activity per week; improves hepatic perfusion.
- Stay hydrated; water helps the liver process metabolites.
- Avoid over‑the‑counter pain relievers like acetaminophen > 2 g daily.
Quick Checklist for Clinicians
- Baseline LFTs before first dose.
- Follow the 2‑week, 4‑week, monthly, then quarterly schedule.
- Know the 3 × ULN and 5 × ULN thresholds.
- Have cholestyramine or activated charcoal on hand for rapid drug removal.
- Document contraception compliance in women of child‑bearing age.
- Reassess hepatic risk when adding new meds.
Frequently Asked Questions
How soon after starting Teriflunomide can liver enzyme spikes appear?
Most elevations show up within the first six weeks, which is why the guideline mandates tests at week 2 and week 4.
Is a mild ALT rise (2 × ULN) a reason to stop treatment?
No. For isolated, asymptomatic rises ≤ 3 × ULN, clinicians usually continue therapy, repeat the test in a week, and address reversible contributors such as alcohol.
What is the fastest way to clear Teriflunomide from the body?
Accelerated elimination with cholestyramine 4 g three times daily (or activated charcoal 50 g three times daily) for 11 days reduces serum levels by over 95 %.
Can I take statins together with Teriflunomide?
Statins are not known to interact significantly with Teriflunomide, but regular LFT monitoring is still advised because both drugs can affect the liver.
What should I do if a patient becomes pregnant while on Teriflunomide?
Immediately start accelerated elimination, confirm drug levels are below 0.02 mg/L, and switch to a pregnancy‑compatible MS therapy.
By staying vigilant with the schedule above, interpreting results wisely, and having a clear action plan, clinicians can keep patients on Teriflunomide safely while protecting liver health.

11 Comments
Tracy O'KeeffeOctober 18, 2025 AT 20:02
Ah, the grandiose theater of liver monitoring-an administrative ballet that masquerades as patient safety. While the EMA and FDA parade their checklists, the real pharmacodynamics of teriflunomide whisper a different truth: hepatotoxicity is seldom the villain, but rather a plot device for paperwork. One could argue that a bi‑weekly LFT schedule is an over‑engineered safety net, more suited to a bureaucratic audit than to clinical insight.
Yet, for the diligent clinician who relishes data, those thresholds (< 3×ULN, >5×ULN) provide a comforting metric, albeit sprinkled with jargon and occasional miss‑spelling of hepatocelllar injury.
In short, embrace the ritual, but remember it’s a performance, not a panacea.
Rajesh SinghOctober 25, 2025 AT 18:42
The ethical responsibility of physicians extends far beyond prescribing a convenient pill; it encompasses a vigilant guardianship over every organ the drug touches, especially the liver.
When teriflunomide is introduced, the clinician must adopt a mindset akin to a steward of a delicate ecosystem, recognizing that hepatic cells, though resilient, are not impervious to chemical assault.
Neglecting the recommended baseline LFTs is tantamount to sailing a ship without a compass, inviting disaster that could have been averted with simple foresight.
Even a modest elevation of ALT to three times the upper limit should trigger a pause, because complacency breeds harm.
The moral imperative demands that we scrutinize concomitant medications, for polypharmacy can amplify hepatic stress in ways that are rarely disclosed in clinical trial abstracts.
Patients deserve transparent discussions about the potential for hepatotoxicity, not a vague reassurance that “it’s rare.”
Educating them on lifestyle modifications-limiting alcohol, adopting a Mediterranean diet, and avoiding excess acetaminophen-transforms passive recipients into active participants in their care.
If a bilirubin surge exceeds two times ULN, the correct course is swift discontinuation, for the cost of a delayed response may be irreversible liver injury.
The accelerated elimination protocol with cholestyramine or activated charcoal, though cumbersome, reflects a commitment to rapid remediation rather than resigned acceptance.
Moreover, the clinician must document each decision meticulously; this is not mere bureaucracy but a safeguard for future accountability and medicolegal protection.
In the context of pregnant patients, the stakes amplify, demanding immediate drug removal and a switch to teratogen‑safe alternatives, underscoring the intersection of reproductive ethics and pharmacology.
Aging patients, whose hepatic perfusion wanes, require even closer surveillance, reminding us that age is not just a number but a physiological modifier.
Finally, the healthcare system should support clinicians with easy access to LFT ordering tools and reminders, reducing reliance on memory alone.
In sum, the paradigm of teriflunomide management is not a rigid algorithm but a moral covenant between physician and patient, rooted in vigilance, education, and swift action when thresholds are breached.
Upholding this covenant preserves not only liver health but the very trust that underpins the therapeutic alliance.
Drew WaggonerNovember 1, 2025 AT 16:22
Monitoring liver enzymes with teriflunomide feels like walking a tightrope, where each weekly LFT is a safety net that keeps us from a fall.
The anxiety of waiting for results is real, yet the structured schedule-weeks 2, 4, then monthly-offers a reassuring rhythm.
If values creep above 3×ULN, a brief pause is prudent, allowing the liver a moment to recover before we press forward.
Ultimately, disciplined vigilance protects both the patient and the clinician’s peace of mind.
Mike HamiltonNovember 8, 2025 AT 15:02
In the grand tapestry of medicine, liver monitoring is but a single thread, yet one that holds together the whole fabric of therapy.
When we check ALT and AST, we are not merely reading numbers; we are listening to the silent whispers of the liver.
A simple repeat in a week can reveal whether a rise was a fleeting surge or a harbinger of deeper trouble.
For older patients, the liver’s cadence may be slower, so we watch a little closer, spacing the tests to catch subtle shifts.
Thus, humble vigilance becomes the philosopher’s stone that turns potential toxicity into safe, sustained care.
Matthew MillerNovember 15, 2025 AT 13:42
Spot on, Mike! Your poetic take reminds us that every lab draw is a chance to keep the engine humming-let’s keep that momentum alive and fire up the clinic schedule.
Linda ANovember 22, 2025 AT 12:22
Rajesh, your moral compass shines bright, yet the shadows of clinical reality whisper a different tale.
In the silent corridors of the liver, enzymes rise and fall like verses in an unfinished poem, demanding patience more than judgment.
While thresholds guide us, the true art lies in discerning the subtle cadence of each patient’s story.
A measured pause, a compassionate conversation, and a steady hand often achieve what fervent admonitions cannot.
Thus, let us balance duty with empathy, honoring both science and the human spirit.
In this equilibrium, the liver finds its safest path.
Joe MooreNovember 29, 2025 AT 11:02
Ever notice how the 2‑week, 4‑week LFT schedule feels less like science and more like a hidden agenda to keep us hooked on lab bills?
Some whisper that pharma lobbies for relentless testing to pad the profit stream, while the real liver might be fine after the first month.
Don’t get me wrong, safety is key, but a skeptics eye wonders why the same drug gets a gentler watch in other countries.
Maybe the truth is buried in the fine print of those EMA guidelines, waiting for a whistleblower.
Poornima GanesanDecember 6, 2025 AT 09:42
Let’s cut through the fluff and get to the crux: teriflunomide’s hepatic risk is quantifiable, not speculative.
First, baseline LFTs set the reference point-no debate there.
Second, the 2‑week and 4‑week checkpoints catch the majority of enzyme spikes, as data show 80 % of elevations appear within six weeks.
Third, the 3×ULN rule is a hard stop; anything above that warrants an immediate repeat in seven days.
If the repeat stays high, a dose hold is the logical next step-nothing mystical about it.
Fourth, a bilirubin rise above 2×ULN is a red flag that overrides all other considerations; the drug must be stopped.
Fifth, accelerated elimination with cholestyramine isn’t a luxury, it’s a necessity to prevent long‑term damage.
Sixth, patients on statins or methotrexate need extra scrutiny, as drug‑drug interactions can amplify hepatotoxic potential.
Seventh, lifestyle counseling-moderate alcohol, Mediterranean diet, regular exercise-acts as a protective buffer.
Finally, documentation isn’t optional; it’s the audit trail that safeguards both patient and practitioner.
Emma WilliamsDecember 13, 2025 AT 08:22
Follow the schedule and keep the liver safe.
Stephanie ZaragozaDecember 20, 2025 AT 07:02
Poornima, your systematic breakdown is immaculate; however, let me emphasize-while the thresholds are clear, the clinical context must never be ignored!!!
In practice, a patient’s comorbidities, medication list, and even stress levels can modulate enzyme dynamics, and those variables deserve equal weight!!!
Thus, while adhering to the protocol, we must also wield clinical judgment as our guiding compass!!!
James MaliDecember 27, 2025 AT 05:42
Another checklist, another hour of paperwork-efficient, yet uninspired.