SAH Treatment: Best Practices and Options
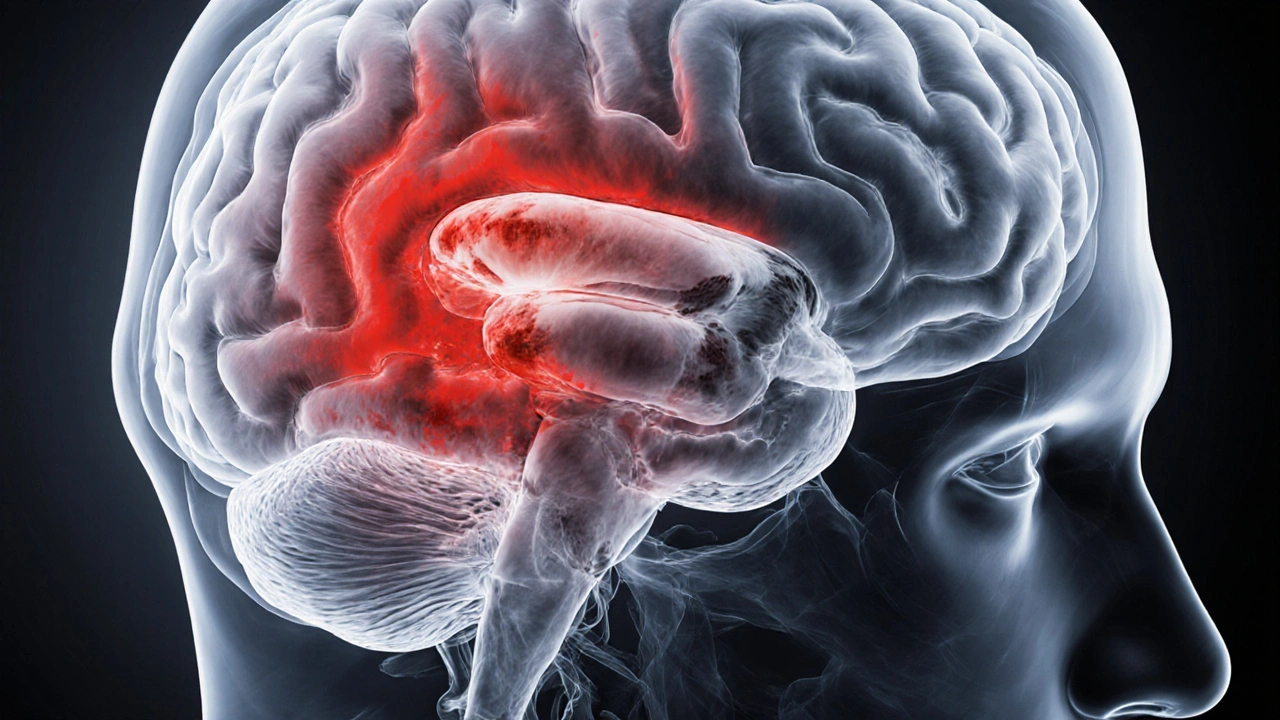
When dealing with SAH treatment, the medical approach to subarachnoid hemorrhage (SAH), a sudden bleed into the space surrounding the brain. Also known as subarachnoid hemorrhage therapy, it aims to stop bleeding, prevent re‑bleed, and limit brain injury. Effective SAH treatment requires rapid diagnosis, early blood‑pressure control, and a plan for securing the bleeding source. This process encompasses Subarachnoid hemorrhage, a type of stroke caused by rupture of a cerebral aneurysm, which can trigger severe headache, loss of consciousness, and a cascade of neurological damage.
Key Components of SAH Care
One of the first decisions in aneurysm repair, the surgical or endovascular process used to seal a ruptured brain aneurysm is whether to clip the aneurysm via open neurosurgery or to coil it through an endovascular route. Both methods aim to isolate the aneurysm from circulation, but they differ in invasiveness, recovery time, and suitability for certain aneurysm shapes. Endovascular coiling, a minimally invasive technique that fills the aneurysm sac with platinum coils has become the go‑to for many patients because it reduces operative trauma and shortens hospital stay. However, complex bifurcation aneurysms may still need a traditional neurosurgical clipping, direct placement of a metal clip on the aneurysm neck to achieve durable closure. The choice between these options influences short‑term complications and long‑term re‑bleed rates.
Pharmacologic support also plays a crucial role. Nimodipine, a calcium‑channel blocker specifically proven to reduce delayed cerebral ischemia after SAH is administered for 21 days to improve neurological outcomes. Studies show that nimodipine lowers the risk of vasospasm, a dangerous narrowing of brain arteries that can occur days after the bleed. Blood‑pressure management, seizure prophylaxis, and fluid balance are other essential pillars. Together, these medical measures illustrate the semantic triple: Effective SAH treatment requires early diagnosis, timely aneurysm repair, and targeted pharmacologic therapy.
Beyond the acute phase, rehabilitation and long‑term monitoring are indispensable. Patients often face cognitive deficits, mood changes, and persistent headaches that need multidisciplinary follow‑up. Imaging follow‑up—usually a CT angiogram or MR angiography—checks for residual aneurysm or new vascular lesions. Lifestyle modifications such as smoking cessation, blood‑pressure control, and regular exercise lower the chance of a second bleed. The combination of rapid intervention, precise surgical or endovascular technique, and diligent medical care forms a cohesive roadmap for anyone navigating SAH treatment. Below you’ll find a curated set of articles that dive deeper into each of these areas, from emergency protocols to the latest advances in coil technology and drug therapy.
Learn how medications like nimodipine, antihypertensives, and antiepileptics manage subarachnoid hemorrhage symptoms, prevent complications, and improve recovery outcomes.