Penicillin Desensitization Eligibility Checker
This tool helps determine if you're eligible for penicillin desensitization based on your allergy history. Penicillin desensitization is only appropriate for certain patients who need penicillin for critical treatment but have a history of mild to moderate reactions.
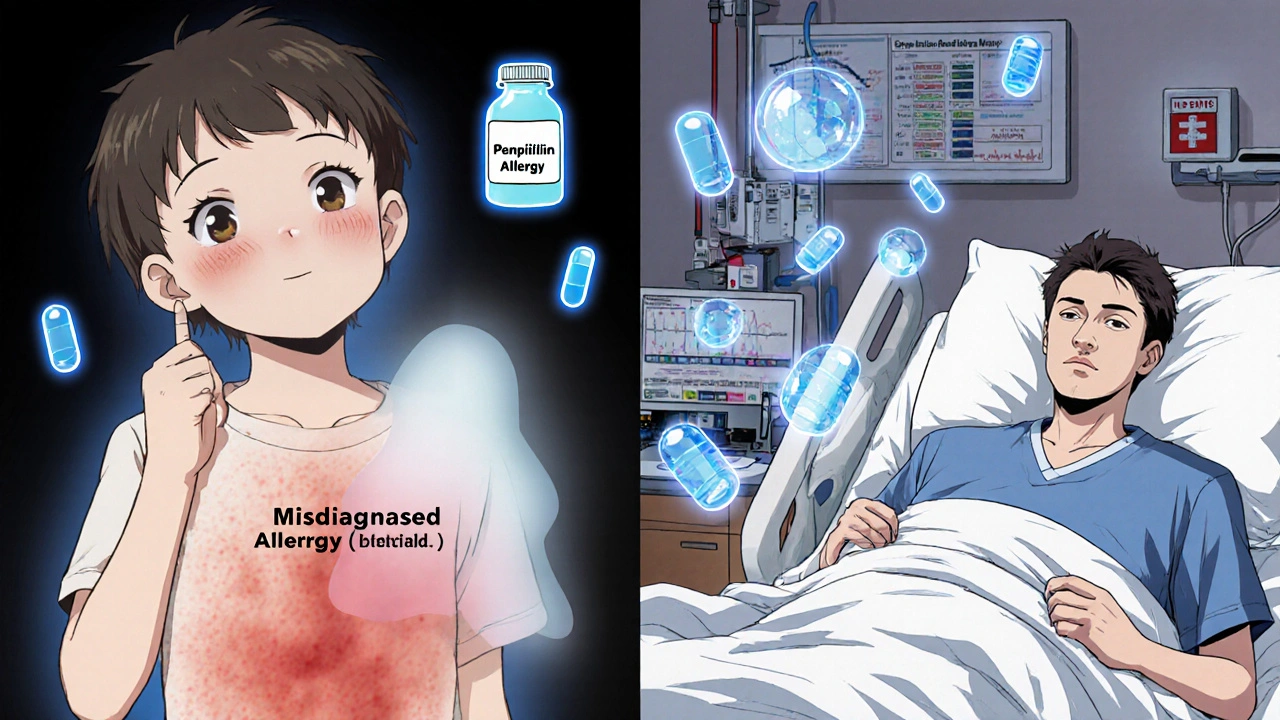
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the catch: 90% of them aren’t. Many were misdiagnosed as kids after a rash, or outgrew the allergy without knowing it. Still, that label sticks-and it’s costing lives, money, and progress in fighting infections.
When someone with a penicillin allergy label needs treatment for something like neurosyphilis, bacterial endocarditis, or group B strep during pregnancy, doctors are forced to use broader-spectrum antibiotics. These drugs are more expensive, less effective, and fuel antimicrobial resistance. That’s where penicillin desensitization comes in-not as a cure, but as a temporary, controlled way to safely give the right antibiotic when there’s no better option.
What Penicillin Desensitization Actually Does
Penicillin desensitization isn’t about fixing your immune system. It doesn’t remove the allergy. Instead, it tricks your body into tolerating penicillin long enough to complete a critical course of treatment. The process involves giving tiny, gradually increasing doses of penicillin over several hours under close medical supervision. Your body doesn’t get a chance to mount a full allergic reaction because the dose never crosses the threshold that triggers one.
This technique has been around since the 1950s, but modern protocols-standardized by hospitals like Brigham and Women’s and updated by Prisma Health in 2024-are far more precise. Today’s methods start with doses so small they’re measured in micrograms, not milligrams. For IV protocols, the first dose might be just 20 units of penicillin, diluted in saline and given slowly. Each next dose doubles the previous one, with 15 to 20 minutes between doses. The whole process usually takes 4 to 6 hours.
Oral desensitization is also used, especially for less urgent cases. It uses longer intervals-45 to 60 minutes between doses-and is often considered safer and easier to manage. But both methods require the same thing: constant monitoring. Vital signs are checked every 15 minutes. Nurses watch for hives, swelling, wheezing, or drops in blood pressure. If any of these happen, the protocol stops immediately.
Who Can and Can’t Get Desensitized
Not everyone with a penicillin allergy label is a candidate. Desensitization is reserved for patients who truly need penicillin-and who have a history of mild to moderate reactions. That means if you had hives, itching, or a mild rash after taking penicillin years ago, you’re likely a good fit.
But if you’ve ever had Stevens-Johnson Syndrome, Toxic Epidermal Necrolysis, or DRESS syndrome after taking penicillin, you’re not eligible. These are life-threatening skin reactions that involve your immune system attacking your own tissues. Desensitization won’t help here-it could kill you.
Another key point: desensitization only works if you keep taking penicillin. Once you stop, the tolerance fades. The effect lasts only 3 to 4 weeks. So if you need another course of penicillin a month later, you’ll have to go through the whole process again. That’s why it’s only done when the antibiotic is essential for a specific, time-limited treatment.
How It’s Done: IV vs. Oral Protocols
There’s no single national protocol. In fact, a 2022 study found 47 different penicillin desensitization protocols across 50 U.S. hospitals. That’s dangerous. Inconsistent methods mean inconsistent safety.
Still, two main approaches dominate: intravenous and oral.
IV desensitization is used for serious infections like endocarditis or syphilis. It allows precise control over dosing and rapid adjustments if a reaction occurs. It’s done in a hospital, often in intensive care or Labor and Delivery for pregnant patients. The starting dose is tiny-sometimes 10^-5 or 10^-6 of the full therapeutic dose. Doses double every 15 to 20 minutes. By the end, you’re receiving the full therapeutic dose. The process takes 4 hours or less.
Oral desensitization is used for less urgent cases or when IV access isn’t ideal. It’s slower-doses are given every 45 to 60 minutes. The starting dose is usually 10 mg or less. About one-third of patients report mild symptoms like itching or flushing, which can be managed with antihistamines. It’s less risky than IV, and studies show it’s just as effective for many conditions.
One thing both methods share: they’re not graded challenges. A graded challenge is when you give a small dose of penicillin to test if someone is still allergic. It’s for people with low-risk histories. Desensitization is for confirmed or strongly suspected allergies. Mixing them up has led to preventable anaphylaxis.
Preparation and Safety Measures
Desensitization isn’t something you do in a clinic. It requires a hospital setting, trained staff, and emergency equipment ready at the bedside. The CDC and AAAAI both say it must be done under allergist supervision.
Before the procedure starts, patients often get premedication:
- Ranitidine (50 mg IV or 150 mg oral)
- Diphenhydramine (25 mg IV or oral)
- Montelukast (10 mg oral)
- Cetirizine or loratadine (10 mg oral)
These are given about an hour before the first penicillin dose to reduce the chance of a reaction. Even with this, minor reactions still happen in about 33% of cases. That’s why nurses are trained to slow the protocol if a rash or flushing appears. Slowing down often stops the reaction before it escalates.
Every dose must be documented. Pharmacy teams prepare specific labels and IV bags with exact concentrations. Nurses sign off on each dose in the electronic medical record. One wrong label, one missed check, and the whole thing can go wrong.
And yes-there’s always a crash cart nearby. Epinephrine, oxygen, IV fluids, and airway tools must be immediately available. Anaphylaxis during desensitization is rare, but when it happens, it’s fast. Teams need to be ready.
Why This Matters Beyond the Individual Patient
Penicillin is cheap. It’s effective. And it’s narrow-spectrum, meaning it kills only the bad bacteria, not the good ones in your gut. When we avoid penicillin because of a mislabeled allergy, we reach for vancomycin, fluoroquinolones, or carbapenems. These drugs are broader, cost more, and drive resistance.
Studies show that patients with a penicillin allergy label pay $3,000 to $5,000 more per hospital stay due to these substitutions. They also have higher rates of C. diff infections, longer hospital stays, and more treatment failures.
The CDC calls penicillin allergy delabeling a “high-impact intervention.” That’s why they’ve funded $15 million in grants since 2020 to help hospitals set up allergy clinics and desensitization programs. The goal? Cut down unnecessary antibiotic use and slow the rise of superbugs.
Right now, only 17% of community hospitals have formal desensitization protocols. Academic centers? Nearly 90%. That gap needs closing. Every hospital that treats infections should be able to offer this.
What Comes Next
The future of penicillin desensitization is about standardization and accessibility. The AAAAI and IDSA are pushing for national protocols. Some hospitals are already integrating desensitization into electronic health records-so when a patient’s allergy is flagged, the system suggests testing or desensitization instead of defaulting to a stronger antibiotic.
Researchers are also exploring whether we can extend the window of tolerance beyond 3-4 weeks. Right now, if you stop penicillin for even a day, you lose the effect. If we could find a way to make the tolerance last longer-maybe by targeting specific immune pathways-we could change how we treat chronic infections.
For now, the best thing you can do if you’ve been told you’re allergic to penicillin is to get tested. Skin testing and blood tests can confirm whether you’re still allergic. If you’re not, you can have the label removed. If you are, and you need penicillin for a serious infection, desensitization is a safe, proven option.
It’s not magic. It’s medicine. And it’s saving lives every day in hospitals that know how to do it right.
Is penicillin desensitization a cure for penicillin allergy?
No, it’s not a cure. Desensitization only temporarily allows your body to tolerate penicillin during a specific treatment. Once you stop taking the drug, the tolerance fades within 3 to 4 weeks. You’ll need to repeat the process if you need penicillin again later.
Can I do penicillin desensitization at home?
Absolutely not. Penicillin desensitization must be done in a hospital under direct medical supervision. It requires continuous monitoring of vital signs, immediate access to emergency equipment, and trained staff who can respond to anaphylaxis. Attempting this outside a controlled setting is extremely dangerous.
What if I had a severe reaction to penicillin years ago?
If your reaction involved blistering skin, peeling skin, fever, or organ involvement-like Stevens-Johnson Syndrome, DRESS, or Toxic Epidermal Necrolysis-you are not a candidate for desensitization. These are life-threatening conditions, and repeating exposure carries a high risk of recurrence. You should avoid all penicillin-class antibiotics permanently.
How long does the entire desensitization process take?
Most IV protocols take about 4 hours to complete, with doses given every 15 to 20 minutes. Oral protocols take longer-usually 6 to 8 hours-because doses are spaced further apart. The goal is to reach the full therapeutic dose safely, without triggering a reaction.
Are there alternatives to penicillin desensitization?
Yes, but they’re not always better. Alternatives include other antibiotics like vancomycin, clindamycin, or fluoroquinolones. But these are broader-spectrum, more expensive, and increase the risk of antibiotic resistance and C. diff infections. For many serious infections, penicillin remains the most effective option-making desensitization the preferred choice when appropriate.
Who should perform penicillin desensitization?
Only trained providers in a hospital setting, ideally with allergist supervision. The CDC and AAAAI require that desensitization be done by teams with specific training and experience. Providers should have completed at least five supervised desensitizations before doing one independently. This isn’t a procedure for general practitioners or emergency rooms without support.

13 Comments
Brad SeymourNovember 7, 2025 AT 09:40
Man, I had no idea so many people get misdiagnosed with penicillin allergies. My cousin got labeled back in 2005 after a rash from amoxicillin, and now she’s stuck with vancomycin every time she gets an infection. It’s wild how much this one label screws people over long-term.
Malia BlomNovember 7, 2025 AT 11:14
So let me get this straight - we’re spending millions to trick people into tolerating a drug they’re allergic to instead of just developing better antibiotics? That’s like putting duct tape on a leaking dam and calling it innovation. The real problem isn’t the allergy, it’s Big Pharma’s failure to innovate past 1940s chemistry.
Erika PuhanNovember 9, 2025 AT 09:00
The methodology here is statistically underpowered. You’re conflating self-reported allergies with clinically validated IgE-mediated reactions. Without skin testing or basophil activation assays, you’re essentially institutionalizing diagnostic error. This protocol is a Band-Aid on a systemic failure of clinical allergy training.
Edward WeaverNovember 10, 2025 AT 14:03
Why are we even doing this? America’s got the best medical tech in the world. If you’re allergic to penicillin, just use one of the 50 other antibiotics we’ve got. Stop coddling people who can’t handle a simple drug. This desensitization crap is just lazy medicine wrapped in a fancy acronym.
Lexi BrinkleyNovember 10, 2025 AT 21:27
OMG this is so important!! 🙌 I work in OB and we do this ALL THE TIME for group B strep. One lady cried because she finally got the right antibiotic after 15 years of being told ‘no penicillin.’ It’s not magic, it’s just… right? 💕
Kelsey VegNovember 11, 2025 AT 22:58
so like… if u got a rash as a kid u rnt actually allergic?? that sounds like bs. my aunt had anaphylaxis and now they wanna just shove penicillin down her throat?? no thanks. i trust my gut more than some hospital protocol.
Alex HarrisonNovember 12, 2025 AT 02:33
I’ve seen this in action at my local hospital. The IV protocol takes about 4 hours, but they start with microgram doses and go slow. Nurses are hyper-vigilant. It’s not perfect, but it’s way better than giving someone vancomycin for syphilis. We’ve saved at least 3 patients from treatment failure this year alone.
Jay WallaceNovember 13, 2025 AT 08:28
It’s astonishing - 47 different protocols across 50 hospitals? This is chaos. In Germany, we have one standardized, evidence-based protocol - enforced by national guidelines. Here? It’s a free-for-all. No wonder there are preventable deaths. This isn’t medicine - it’s medical anarchy.
Alyssa FisherNovember 13, 2025 AT 13:20
It’s funny how we treat allergies like a binary - you’re either allergic or you’re not. But biology doesn’t work that way. Immune responses are dynamic, context-dependent, and often fade over time. The real tragedy isn’t the allergy - it’s that we stopped asking questions. We stopped listening to patients. We just stamped a label and walked away.
Alyssa SalazarNovember 15, 2025 AT 10:31
Let’s be real - desensitization is only viable because we’ve failed at public health education. If we taught people that rashes ≠ allergy, and that 90% outgrow it, we wouldn’t need this whole system. It’s a workaround for a preventable problem. We’re treating symptoms, not root causes.
Beth BanhamNovember 15, 2025 AT 13:12
Just wanted to say thank you for writing this. My sister went through desensitization last year for endocarditis. It was scary, but it worked. She’s fine now. I wish more people knew this was an option.
Brierly DavisNovember 17, 2025 AT 13:09
For anyone reading this - if you think you’re allergic to penicillin, get tested. Seriously. It’s a simple skin prick test. Takes 20 minutes. Could save you thousands and maybe even your life. You’ve got nothing to lose and everything to gain. 💪
Amber O'SullivanNovember 18, 2025 AT 05:09
Penicillin is cheap and effective. We’re using tank missiles to kill ants. This isn’t innovation - it’s just laziness dressed up as science. Fix the system not the symptom