Ethnicity and Drug Response: How Genetics Influence Medication Effectiveness
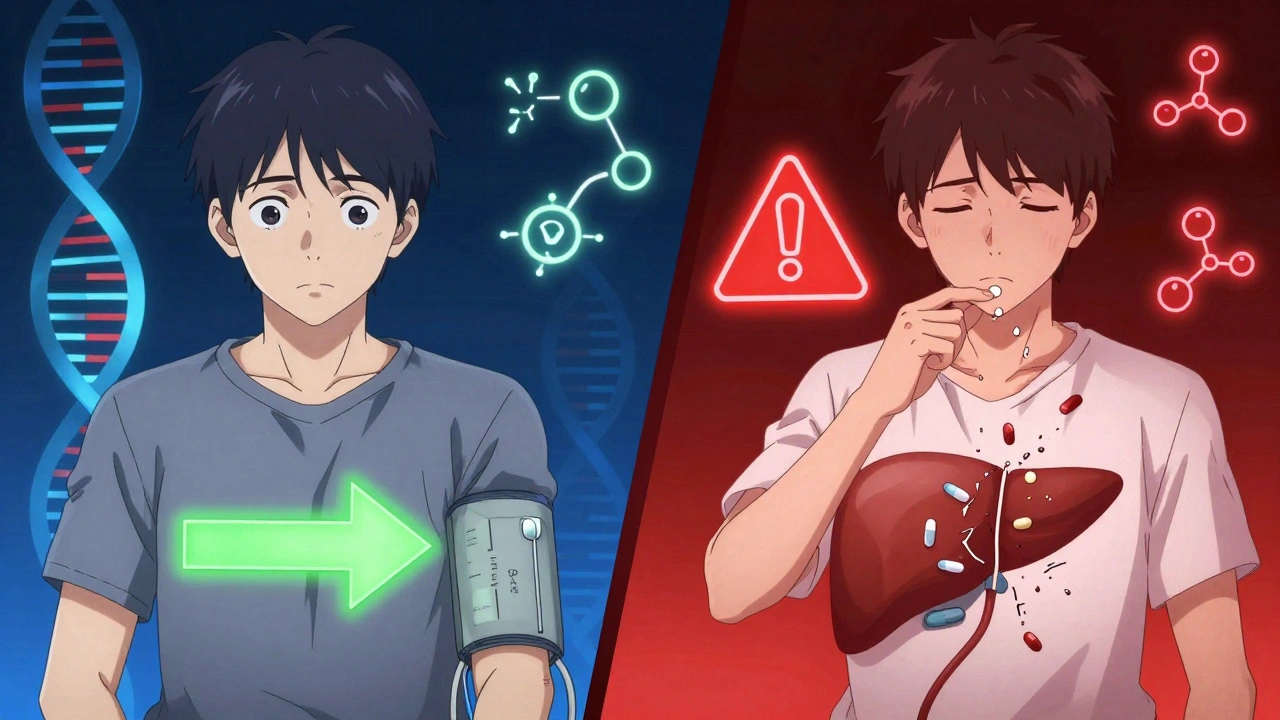
When you take a pill, your body doesn’t treat it the same way everyone else’s does. ethnicity and drug response, how genetic differences tied to ancestral background affect how medicines work in the body. Also known as pharmacogenomics, it’s not about race as a social idea—it’s about inherited biology that changes how drugs are absorbed, broken down, and cleared. Someone of East Asian descent might need a lower dose of a blood thinner because their liver processes it faster. Someone of African descent might respond better to certain blood pressure meds than others. These aren’t guesses—they’re patterns backed by real data from clinical studies and population-level drug trials.
pharmacogenomics, the study of how genes affect a person’s response to drugs explains why one person gets sick from a standard dose while another feels nothing. It’s tied to enzymes like CYP2D6 and CYP2C19, which break down meds in the liver. These enzymes vary wildly across populations. For example, up to 25% of East Asians have a version of CYP2C19 that makes them poor metabolizers of clopidogrel, a common heart drug—meaning it won’t work well for them. Meanwhile, about 5% of Caucasians have the same issue. That’s why doctors in some countries now test for these variants before prescribing.
It’s not just about metabolism. genetic variation, differences in DNA that affect how drugs bind to targets in the body can change how well a drug even works. A diabetes drug called metformin might lower blood sugar better in people of European descent than in those of African descent, not because of diet or lifestyle alone—but because of a gene variant that affects how the drug enters cells. Even side effects like skin rashes from certain antibiotics are more common in specific groups. One study found that Han Chinese patients had a 100x higher risk of a deadly skin reaction to carbamazepine than other groups, simply because of a genetic marker.
These aren’t rare exceptions. They’re routine differences that affect millions. And yet, most prescriptions still ignore this. Doctors often give the same dose to everyone, assuming one-size-fits-all works. But if you’re part of a group where a drug is known to be less effective—or more dangerous—it matters. You deserve to know if your ancestry could be influencing your treatment.
What you’ll find in the posts below are real, practical insights into how your body handles drugs. From liver metabolism to drug interactions, these articles break down the science behind why some people react differently. You’ll learn how to spot when your medication might not be working as expected—and what to ask your doctor next.
Ethnicity influences how your body processes medications due to genetic differences in drug metabolism. Learn how CYP450 enzymes, HLA variants, and pharmacogenomics are changing prescribing practices to improve safety and effectiveness.