Drug Dose Calculator
Your body processes drugs differently based on age, kidney function, and other factors. This calculator estimates adjusted doses for common medications using pharmacokinetic principles.
Ever taken a pill and wondered why it worked for your friend but gave you a headache? Or why your grandma needs a lower dose of the same medicine you take? It’s not luck. It’s not magic. It’s pharmacokinetics-the science of how your body moves, changes, and gets rid of drugs. And if you don’t understand it, you’re flying blind when it comes to side effects.
What Happens When You Swallow a Pill?
Your body doesn’t treat every drug the same. A painkiller you take on an empty stomach might hit your bloodstream faster than one taken after a big meal. That’s because of absorption-the first step in what’s called the ADME process: Absorption, Distribution, Metabolism, Excretion.When you swallow a tablet, it breaks down in your stomach. Most drugs slip through the lining of your intestines into your blood. But not all of it makes it. About 40-60% of oral drugs get broken down by your liver before they even reach your bloodstream. This is called first-pass metabolism. That’s why some pills have to be taken in higher doses than injections-because your body filters out a chunk before it can do its job.
Injecting a drug straight into your vein? That’s 100% bioavailability. No filtering. No waiting. But even then, your body doesn’t just let the drug hang out. It’s already moving on to the next step.
Where Does the Drug Go After It Enters Your Blood?
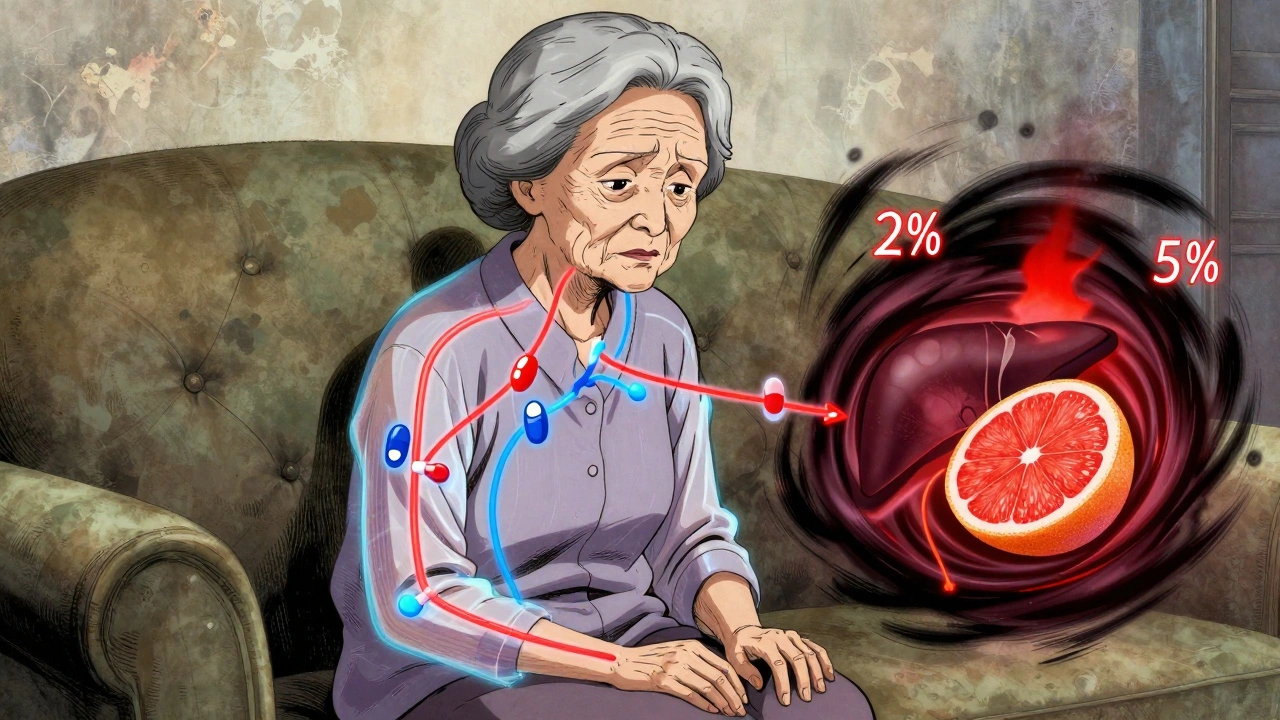
Once in your bloodstream, the drug starts spreading. Some drugs stay mostly in your blood. Others dive deep into your fat, brain, or muscles. Scientists measure this spread with something called the volume of distribution (Vd). A low Vd means the drug sticks close to your blood. A high Vd? It’s everywhere-your tissues, your organs, even your fat cells.Take warfarin, a blood thinner. About 98% of it clings to proteins in your blood. Only 2% is free to work. That tiny bit is what prevents clots-but also what causes bleeding if the dose is too high. If you’re sick, dehydrated, or on another drug that pushes warfarin off those proteins, that 2% can suddenly jump to 5%. That’s when things go wrong.
And then there’s the blood-brain barrier. Some drugs can’t cross it. Others slip through easily. That’s why some antidepressants cause drowsiness-they’re getting into your brain. Others don’t. It’s not about strength. It’s about chemistry.
Your Liver: The Drug Transformer
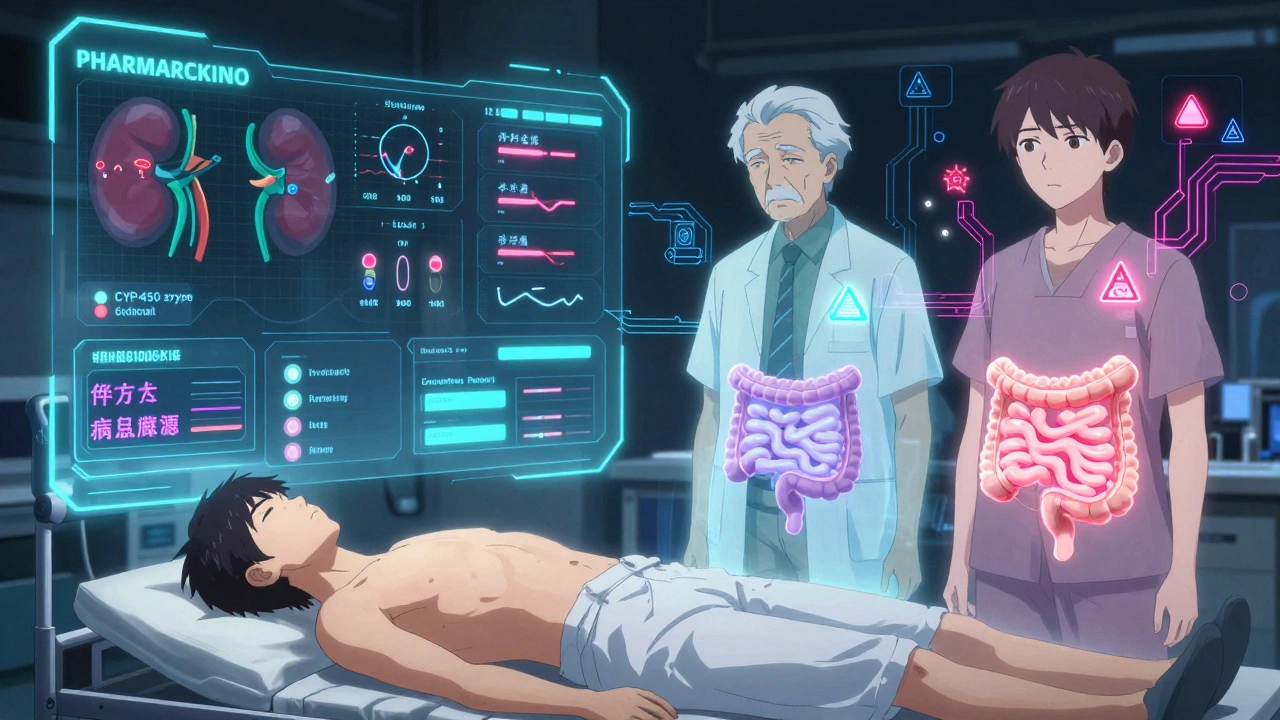
Your liver doesn’t just detoxify alcohol. It’s the main factory that turns drugs into forms your body can flush out. This is metabolism-and it’s done mostly by a family of enzymes called Cytochrome P450 (CYP).CYP3A4 alone handles about half of all prescription drugs. That includes statins, antibiotics, and even some heart medications. But here’s the catch: your genes decide how fast or slow your CYP enzymes work. About 3-10% of white Europeans are slow metabolizers of CYP2D6. That means codeine, which needs to be converted into morphine to work, doesn’t help them at all. Meanwhile, ultra-rapid metabolizers turn it into morphine too fast-and risk overdose.
And it’s not just genetics. Grapefruit juice? It blocks CYP3A4. One glass can make your cholesterol drug 3-5 times stronger. Clarithromycin, a common antibiotic, does the same. Combine it with simvastatin, and your risk of muscle damage jumps from 0.04% to 0.5%. That’s not rare. That’s predictable.
How Your Body Gets Rid of Drugs
Most drugs leave through your kidneys. Your kidneys filter about 125 milliliters of blood per minute. That’s your glomerular filtration rate (GFR). Normal? 90-120 mL/min. If you’re over 70? It’s probably down to 60. If you have kidney disease? It could be below 15.That’s why vancomycin, an antibiotic, can wreck kidneys in older patients. If you’re on the standard dose and your kidneys can’t clear it fast enough, it builds up. One patient in a Reddit thread had their creatinine spike from 1.2 to 3.4 mg/dL after just a few days-classic toxicity. The dose was right for a young, healthy person. Not for someone with aging kidneys.
Some drugs are cleared by the liver. Others by bile. A few even get excreted in sweat or breath. But kidneys? They’re the main exit ramp. And if you’re dehydrated, on diuretics, or have high blood pressure, your GFR drops. Your drug sticks around longer. Side effects get worse.
Why Side Effects Aren’t Random
Side effects aren’t just bad luck. They’re usually the direct result of drug levels being too high-or staying too long.Phenytoin, an anti-seizure drug, has a narrow window. At 10-20 mcg/mL, it works. Above 20, you start shaking, vomiting, even losing coordination. At 30? You could slip into a coma. That’s not an allergic reaction. That’s pharmacokinetics. Your liver can’t keep up. Your kidneys are slowing down. Or you started taking another drug that blocks its breakdown.
Even the metabolites matter. Diazepam, a common anxiety pill, turns into desmethyldiazepam. That metabolite has a half-life of up to 100 hours. In a 25-year-old? No big deal. In a 78-year-old with slower liver function? It builds up. They feel dizzy. They fall. That’s not aging-it’s pharmacokinetics.
And then there’s the gut. New research shows your gut bacteria can change how drugs work. One study found 15-20% of oral drugs are altered by microbes before they’re even absorbed. That’s why two people taking the same pill can have totally different results. It’s not just genes. It’s your microbiome.
Who’s at Highest Risk?
Three groups get hit hardest by pharmacokinetic surprises:- Older adults: Liver and kidney function drop 30-50% after 65. They’re 3 times more likely to have a bad reaction.
- People with kidney or liver disease: Even mild impairment can double drug levels.
- People on 5+ medications: One drug can block the enzyme that breaks down another. That’s how 20-30% of serious side effects happen.
And here’s the kicker: doctors don’t always check. A Mayo Clinic survey found 42% of people who had bad reactions had at least one of these risk factors-but it wasn’t considered when they were prescribed the drug.
What Can You Do?
You can’t control your genes. But you can control what you tell your doctor.- Know your meds. Write down every pill, supplement, and herb you take-even “natural” ones. St. John’s Wort can knock out 30% of antidepressants.
- Ask about kidney/liver function. If you’re over 65 or have high blood pressure, diabetes, or heart failure, ask: “Should my dose be adjusted?”
- Watch for interactions. Grapefruit juice? Avoid it if you’re on statins, blood pressure meds, or immunosuppressants. Alcohol? It slows down liver metabolism. Even caffeine can interfere with some asthma drugs.
- Track side effects. Did you start feeling foggy after a new pill? Write it down. Bring it up. That’s not being paranoid. That’s being smart.
Therapeutic drug monitoring-testing blood levels-isn’t just for hospitals. It’s becoming more common for drugs like warfarin, lithium, and epilepsy meds. If you’re on one of these, ask if a blood test is needed. It’s not expensive. It’s life-saving.
The Future: Personalized Dosing
We’re moving away from “one-size-fits-all” dosing. AI tools like DoseMeRx now use your age, weight, kidney function, and genetics to calculate your perfect dose for vancomycin-cutting errors by 62%. The FDA cleared it in 2021. It’s not sci-fi. It’s here.And the FDA now requires genetic testing for 28 drugs. Abacavir? Test for HLA-B*5701 before you take it, or you risk a deadly skin reaction. Clopidogrel? If you’re a poor CYP2C19 metabolizer, it won’t work. Your doctor needs to know.
By 2030, we could cut emergency visits from drug side effects by more than half. But only if we start treating pharmacokinetics like the science it is-not an afterthought.
What does pharmacokinetics mean?
Pharmacokinetics is the study of how your body absorbs, distributes, metabolizes, and excretes a drug. It’s often summed up as “what your body does to the drug,” as opposed to pharmacodynamics, which is “what the drug does to your body.”
Why do some people have worse side effects than others?
It’s mostly due to differences in how their bodies process drugs. Genetics affect liver enzymes, age impacts kidney and liver function, and other medications can block or speed up drug breakdown. Even diet and gut bacteria play a role. Two people taking the same pill can have completely different experiences.
Can drinking grapefruit juice really change how my medicine works?
Yes. Grapefruit juice blocks an enzyme in your liver called CYP3A4, which breaks down many common drugs. This can cause drug levels to spike-sometimes by 3 to 5 times. It’s dangerous with statins, blood pressure meds, and immunosuppressants. Always check your medication guide or ask your pharmacist.
Do I need blood tests to check my drug levels?
Not always, but for certain drugs like warfarin, lithium, phenytoin, or vancomycin, yes. These have narrow safety margins-too little doesn’t work, too much is toxic. Blood tests help doctors adjust your dose safely. Ask if it’s recommended for your medication.
Why do older adults get more side effects from drugs?
As we age, our liver processes drugs 30-50% slower, and our kidneys filter them 30-40% less efficiently. That means drugs stay in the body longer and build up to higher levels. Older adults also tend to take more medications, increasing the chance of dangerous interactions.
Can my gut bacteria affect how drugs work?
Yes. Recent research shows gut bacteria can break down or activate up to 20% of oral drugs before they’re absorbed. This could explain why some people don’t respond to certain medications-even when their genetics and organ function look normal. It’s a growing area of study.


10 Comments
Queenie ChanDecember 9, 2025 AT 13:23
Okay, but have you ever taken a pill and felt like your body just said, 'Nah, I'm not doing this today'? Like, I took melatonin and ended up dreaming about flying squirrels in a tuxedo. Pharmacokinetics is wild-your gut bacteria might be throwing a rave while your liver naps. I once asked my pharmacist if my kombucha was interfering with my blood pressure med. She laughed, then Googled it. Turns out, yes. It was. I’m now a convert to the gospel of 'ask your pharmacist, not Google.'
Jack ApplebyDecember 10, 2025 AT 17:11
Let’s be precise: the article misrepresents the concept of bioavailability. It’s not merely '40-60% lost to first-pass metabolism'-that’s an oversimplification. The hepatic extraction ratio, not a static percentage, governs this. And CYP3A4 inhibition by grapefruit? The furanocoumarins irreversibly inhibit the enzyme, requiring de novo synthesis. This isn’t 'one glass makes it 3x stronger'-it’s a pharmacokinetic cascade with nonlinear dynamics. If you’re prescribing statins, you’re either clinically competent or dangerously negligent. The FDA’s 28-drug genetic mandate? Long overdue. The rest of the world is still in the Dark Ages.
Frank NouwensDecember 11, 2025 AT 03:48
Really appreciated this breakdown. I’m a nurse and see this every day-older patients on five meds, no one checking kidney function. I had a patient last month on simvastatin and clarithromycin. Got admitted with rhabdo. We missed the interaction because the script auto-filled. This isn’t just science-it’s patient safety. If you’re on more than three meds, ask your doc: 'Could any of these be talking to each other?' It’s a simple question that saves lives.
Michelle EdwardsDecember 12, 2025 AT 14:14
You’re not alone if you’ve ever felt like your body is a mystery box of reactions. I used to think I was 'just sensitive' to meds-turns out, I’m a slow CYP2D6 metabolizer. Took me years to figure it out. But here’s the good news: once you know how your body works, you can speak up. Write down what you feel. Bring it to your doctor. You’re not being dramatic-you’re being your own best advocate. And yes, grapefruit juice is a sneaky little saboteur. I stopped it cold. My cholesterol dropped 20 points. No meds changed. Just juice gone.
Sarah CliffordDecember 13, 2025 AT 20:18
So you’re telling me my grandma’s dementia isn’t aging-it’s just her meds piling up like dirty laundry? And grapefruit juice is basically poison now? I’m never eating fruit again. Also, why do doctors still write prescriptions like they’re using a typewriter? Someone needs to build an app that auto-blocks bad combos. I’d pay for that.
Regan MearsDecember 13, 2025 AT 23:40
Thank you for writing this. Honestly, I’ve been terrified to take anything new since my dad had a bad reaction to a statin. I didn’t know it was about metabolism, not 'bad luck.' I just thought I was broken. But now I know: it’s biology. It’s not me. I asked my doctor for a CYP2C19 test after my clopidogrel didn’t work-turns out I’m a poor metabolizer. They switched me. I feel like a new person. You’re not weird for asking questions. You’re smart. And you deserve to feel safe in your own skin.
Ben GreeningDecember 14, 2025 AT 03:07
Pharmacokinetic variability is a well-documented phenomenon in clinical pharmacology literature since the 1970s. The article accurately reflects established principles. However, the omission of renal clearance equations (e.g., Cockcroft-Gault) and the lack of reference to therapeutic drug monitoring guidelines (e.g., from the American Society of Health-System Pharmacists) limits its utility for clinical application. The integration of pharmacogenomics into primary care remains underutilized despite robust evidence.
Nikki SmellieDecember 14, 2025 AT 14:11
Wait… so the government is using your DNA to control your meds? And they’re testing for HLA-B*5701? That’s the same gene they use to track immigrants. Are they building a pharmacological surveillance state? I read that gut bacteria are being modified by 5G signals. That’s why my probiotics don’t work anymore. They’re injecting microchips into your pills. I know someone who got a rash after taking a vitamin. They disappeared three days later. The FDA is complicit. Ask yourself: who benefits if you’re always sick? I’ve stopped all meds. I drink lemon water. I’m 92% healed. 🤔
Stephanie MailletDecember 15, 2025 AT 05:51
It’s fascinating, isn’t it? We treat our bodies like machines-pop a pill, get a result-but the truth is, we’re ecosystems. A single pill doesn’t just interact with enzymes-it interacts with trillions of microbes, with decades of diet, with trauma, with sleep, with silence. Pharmacokinetics isn’t just science; it’s poetry written in biochemistry. We’re not broken when drugs don’t work. We’re just complex. Maybe the real problem isn’t the medicine-it’s the assumption that one size fits all. Maybe we need to stop trying to fix people, and start listening to them. Not just their symptoms. Their stories.
Kaitlynn nailDecember 15, 2025 AT 08:50
So… my body’s just a glitchy iPhone? And grapefruit is the iOS update that bricked it? Cool. I’ll just keep taking my vitamins and ignoring the label. 🙃