Migraine Treatment Selector
Do you have heart disease, uncontrolled hypertension, or recent stroke?
How quickly do you need relief?
Have you experienced chest tightness or tingling with Imitrex (Sumatriptan)?
How many migraine days do you have per month?
Did you know that more than 15% of adults in the UK suffer from migraines, and nearly half of them never find a drug that stops the pain fast enough? If you’ve tried Imitrex and wonder whether a different pill might work better, you’re not alone. Below we break down Imitrex (sumatriptan) side‑by‑side with the most common alternatives, so you can decide which option matches your migraine pattern, health profile, and lifestyle.
What is Imitrex (Sumatriptan) and how does it work?
Imitrex is the brand name for sumatriptan, a selective serotonin (5‑HT1B/1D) receptor agonist that narrows dilated cranial blood vessels and blocks pain pathways in the brainstem. It belongs to the triptan class, the first line of prescription treatment for moderate‑to‑severe migraine attacks.
After a migraine begins, taking Imitrex within the first hour usually gives relief within 30‑60 minutes. The drug is available as a 25‑mg tablet, a 6‑mg subcutaneous injection, and a 6‑mg nasal spray, giving patients flexibility based on how quickly they need relief.
Top alternatives to Imitrex
While Imitrex remains the most prescribed triptan in the UK, several newer options compete on speed of onset, side‑effect profile, and suitability for patients with cardiovascular risk. Below are the most widely used alternatives as of 2025.
- Rizatriptan - a rapid‑acting triptan often taken as a 10‑mg tablet; marketed as Maxalt.
- Zolmitriptan - available in 2.5‑mg oral tablets and a 5‑mg nasal spray; known for fast nasal absorption.
- Naratriptan - the longest‑acting triptan (50‑mg tablet), useful for prolonged attacks.
- Eletriptan - 40‑mg tablet with a slightly higher efficacy rating in clinical trials.
- Almotriptan - 12.5‑mg tablet noted for a lower side‑effect burden.
- Lasmiditan - a serotonin 5‑HT1F agonist that works without vasoconstriction, ideal for patients with heart disease.
- Ubrogepant - a CGRP receptor antagonist (gepant) taken as a 50‑mg tablet, safe for vascular patients.
- Erenumab - a monoclonal antibody injected once a month that blocks CGRP receptors, used for preventive therapy.
Head‑to‑Head Comparison
| Medication | Class | Typical Dose | Onset (minutes) | Duration of Relief | Common Side Effects | Cardiovascular Contra‑indication? |
|---|---|---|---|---|---|---|
| Imitrex (Sumatriptan) | Triptan (5‑HT1B/1D) | 25mg tablet / 6mg injection / 6mg nasal spray | 30‑60 | 4‑6hours | Chest tightness, tingling, nausea | Yes - avoid in uncontrolled hypertension, coronary artery disease |
| Rizatriptan | Triptan | 10mg tablet | 20‑40 | 4‑8hours | Dizziness, dry mouth | Yes |
| Zolmitriptan | Triptan | 2.5mg tablet / 5mg nasal spray | 15‑30 (nasal) | 4‑6hours | Urinary retention, fatigue | Yes |
| Lasmiditan | 5‑HT1F agonist | 50‑100mg tablet | 30‑45 | 6‑12hours | Drowsiness, paresthesia | No - no vasoconstriction |
| Ubrogepant | CGRP receptor antagonist (gepant) | 50mg tablet | 30‑60 | 8‑12hours | Dry mouth, nausea | No - vascular‑safe |
| Erenumab | CGRP monoclonal antibody (preventive) | 70‑140mg subcutaneous injection (monthly) | N/A (prevention) | Months of reduction in attack frequency | Injection site reactions, constipation | No - safe for heart patients |

Choosing Imitrex or an Alternative: Practical Considerations
Deciding which drug to keep in your migraine kit isn’t just about numbers on a table; your personal health history, attack pattern, and how quickly you need relief all matter.
- Speed of onset - If you often feel the migraine front‑load within 30minutes, a nasal spray (zolmitriptan) or an injectable (sumatriptan) may be the best bet.
- Frequency of attacks - For patients with more than four attacks a month, a preventive option like erenumab can cut overall drug load and reduce reliance on acute meds.
- Cardiovascular risk - Anyone with a history of heart disease, uncontrolled hypertension, or stroke should avoid triptans. Lasmiditan or the gepants (ubrogepant, rimegepant) provide migraine relief without vessel constriction.
- Side‑effect tolerance - If you experience chest tightness or tingling with sumatriptan, switching to almotriptan (lower side‑effect incidence) or a non‑triptan option may improve adherence.
- Cost and reimbursement - In the UK, many triptans are available on the NHS with a prescription charge, while newer gepants may require private funding. Check your local formulary and private insurance coverage.
Safety, Interactions, and Contra‑indications
All migraine drugs have a safety checklist. Below is a quick cheat‑sheet you can keep on your phone.
- Imitrex (Sumatriptan): Avoid if you take MAO‑B inhibitors, ergot alkaloids, or have uncontrolled cardiac disease. Do not exceed 200mg per day.
- Rizatriptan, Zolmitriptan, Naratriptan, Eletriptan, Almotriptan: Same class warnings as sumatriptan; watch for drug interactions with SSRIs/SNRIs (serotonin syndrome risk).
- Lasmiditan: No vasoconstriction, but should not be taken with alcohol or other CNS depressants due to drowsiness risk.
- Ubrogepant: Safe with most cardiovascular meds, but avoid strong CYP3A4 inhibitors (e.g., clarithromycin) that raise ubrogepant levels.
- Erenumab: Injection site infection is rare; monitor for constipation and blood pressure changes.
If you’re pregnant, nursing, or planning surgery, always discuss migraine meds with your GP or neurologist before making changes.
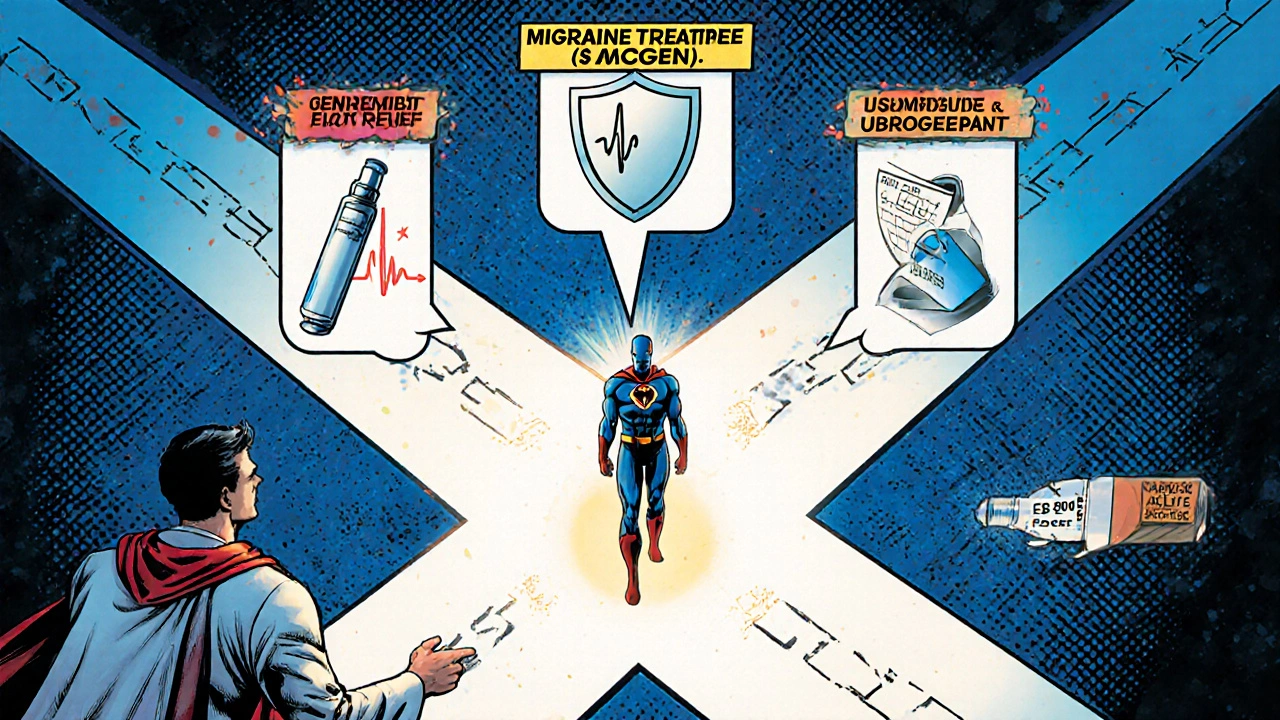
Putting It All Together: A Quick Decision Tree
- Do you have any heart disease, uncontrolled hypertension, or recent stroke?
- Yes → Skip triptans. Consider lasmiditan, ubrogepant, or a preventive CGRP therapy.
- No → Continue to step 2.
- Do you need relief within 30minutes?
- Yes → Nasal spray (zolmitriptan) or subcutaneous sumatriptan.
- No → Oral tablets (rizatriptan, eletriptan, almotriptan) are fine.
- Do you experience chest tightness or tingling with sumatriptan?
- Yes → Switch to almotriptan or try a non‑triptan option.
- No → Imitrex remains a solid first‑line choice.
- Are you having >4 migraine days per month?
- Yes → Discuss a preventive CGRP monoclonal antibody (erenumab) or daily gepant (rimegepant).
- No → Stick with acute abortive meds.
Frequently Asked Questions
Can I use Imitrex together with an over‑the‑counter painkiller?
Yes, most doctors recommend a simple analgesic like paracetamol or ibuprofen alongside sumatriptan to tackle the pain and inflammation. Avoid combining with other triptans or ergot derivatives.
How many times can I take Imitrex in a single day?
The maximum daily dose is 200mg (usually four 25‑mg tablets or two 6‑mg injections). Exceeding this raises the risk of cardiovascular side effects and medication overuse headache.
Is lasmiditan safe if I have high blood pressure?
Lasmiditan does not cause vasoconstriction, so it’s generally considered safe for patients with hypertension. However, you should still discuss any new medication with your GP.
Why do some people get a “post‑dose” migraine after taking sumatriptan?
That's called medication‑overuse headache. If you use triptans more than ten days a month, the brain can become dependent on the drug, leading to rebound pain. Switching to a preventer or spacing out doses can help.
Are the newer CGRP antibodies covered by NHS prescriptions?
In many UK centres, CGRP monoclonal antibodies are prescribed for patients who have failed at least two oral preventives. Eligibility varies by Clinical Commissioning Group, so ask your neurologist for a referral.


10 Comments
Emily RankinOctober 16, 2025 AT 19:43
When you stare at the endless horizon of a migraine, the mind can become a storm in itself. Imitrex, with its swift action, feels like a lighthouse cutting through the fog, offering a promise of calm. Yet the choice of medication is not merely a chemistry lesson; it’s a dialogue with your own resilience. If the headache strikes before you can reach the bathroom, a nasal spray or injection can be a lifeline. For those who enjoy the slower rhythm of a tablet, the trade‑off is a slightly longer wait for relief. Remember, every successful abortive therapy is a small victory that builds confidence for the next bout. Keep experimenting with what fits your rhythm, and you’ll find a personal symphony of relief.
Rebecca MitchellOctober 17, 2025 AT 23:30
Imitrex works but you’re overthinking it
Roberta MakaravageOctober 19, 2025 AT 03:16
🚨 Fact check: most triptans, including Imitrex, share the same vasoconstrictive risk, so you can’t claim one is magically safe for everyone. If you have uncontrolled hypertension, using any triptan is ethically irresponsible because you’re flirting with a potential heart attack. The newer CGRP‑targeted drugs, like ubrogepant or erenumab, are scientifically proven to avoid that danger, making them the morally superior choice for high‑risk patients. 😇 Stay informed, question the “one‑size‑fits‑all” narrative, and demand evidence‑based prescriptions from your doctor.
Katie HenryOctober 20, 2025 AT 07:03
Dear colleagues, it is imperative to underscore the significance of aligning migraine pharmacotherapy with individual cardiovascular profiles. In cases where vasoconstriction presents a contraindication, agents such as lasmiditan or gepants should be considered foremost. Moreover, adherence to dosage limits-specifically the 200 mg daily ceiling for sumatriptan-remains a cornerstone of patient safety. I encourage all practitioners to engage in thorough risk‑benefit discussions, thereby fostering informed consent and optimal therapeutic outcomes.
CHIRAG AGARWALOctober 21, 2025 AT 10:50
Triples are overrated.
genevieve gaudetOctober 22, 2025 AT 14:36
i totally get u but like in the UK they sometimes get sumatriptan for cheap 🤷♀️ and it's def not as pricey as ubrogepant lol
Tom GreenOctober 23, 2025 AT 18:23
Roberta, you raise solid points about safety, and I’d add that insurance coverage often dictates what’s actually accessible to patients. While CGRP therapies are promising, many folks still rely on generics because of cost constraints. It helps to guide them toward the most effective option within their budget, perhaps starting with a trial of a lower‑dose triptan before moving to newer agents.
Winston BarOctober 24, 2025 AT 22:10
Honestly, all these fancy new meds are just marketing hype. I’ve been using plain Imitrex for years and it still does the job.
Russell AbelidoOctober 26, 2025 AT 01:56
It’s understandable to feel loyal to a medication that has served you well over time, especially when you’ve built a routine around it. However, clinging to familiarity can sometimes mask the subtle decline in efficacy that many patients experience after prolonged use. Clinical studies have shown that medication‑overuse headache can emerge after ten or more days of triptan use per month, gradually eroding the therapeutic benefit. Moreover, the vascular contraindications associated with sumatriptan remain a silent risk, even for individuals who consider themselves healthy. While you may not have witnessed a heart‑related event yet, the underlying mechanism of vasoconstriction can still tax the endothelial lining over years. Newer therapies such as lasmiditan or the gepants deliberately avoid this pathway, offering comparable relief without the same cardiovascular footprint. For patients with evolving risk factors-like an emerging hypertension diagnosis-making the switch proactively can be a preventative measure rather than a reactionary one. Additionally, the side‑effect profile of Imitrex, including chest tightness and tingling, can be distressing and may diminish quality of life. Alternatives like almotriptan often present a milder side‑effect burden, which can improve adherence. From a pharmacoeconomic perspective, while brand‑name CGRP antibodies may carry a higher upfront cost, the reduction in emergency visits and lost workdays can offset expenses in the long run. Think of migraine management as a dynamic journey; your treatment arsenal should evolve as your body does. Embracing newer options does not diminish the value of Imitrex; it simply adds flexibility to your toolkit. If you decide to explore a switch, coordinate closely with your neurologist to ensure proper titration and monitoring. Ultimately, the goal is to preserve your ability to function without the looming fear of a cardiovascular event. 😊
Steve HolmesOctober 27, 2025 AT 04:43
Wow, Russell-what a comprehensive rundown!!! I love how you highlighted both the physiological and economic angles; it really paints a full picture!!! One thing I’d add is the importance of patient education on proper dosing schedules-over‑use can sneak up on anyone!!! Also, let’s not forget that individual variability means some patients may still respond best to Imitrex despite the risks!!! So, a balanced, personalized approach remains key!!!