Triptan & Antidepressant Safety Checker
Medication Interaction Checker
This tool is based on evidence from over 61,000 patients and medical guidelines that confirm triptans and SSRIs/SNRIs are safe together. The FDA warning is outdated and based on theory, not real-world evidence.
How this works
This tool is based on 17 years of clinical data showing no cases of serotonin syndrome with triptans and SSRIs/SNRIs. The FDA warning was based on theoretical risk, not evidence from real patients.
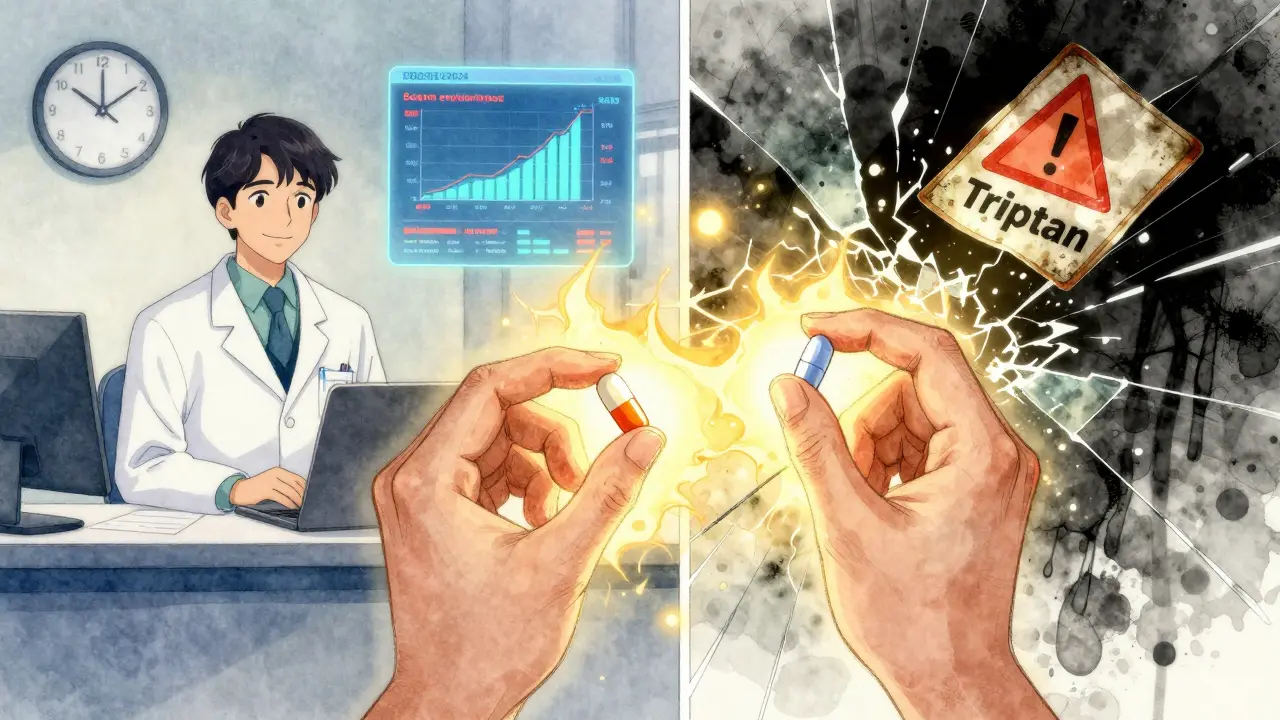
For over a decade, patients with migraines who also take antidepressants have been told they can’t use triptans - the most effective acute migraine treatment - because of a supposed risk of serotonin syndrome. It’s a warning that’s been printed on prescription labels, shouted by pharmacy alert systems, and repeated by well-meaning doctors. But here’s the reality: triptans and SSRIs together are not causing serotonin syndrome. Not in real life. Not in thousands of patients. Not even close.
Where the Fear Came From
In 2006, the U.S. Food and Drug Administration (FDA) issued a safety alert. It said combining triptans like sumatriptan or rizatriptan with SSRIs like sertraline or fluoxetine might cause serotonin syndrome - a rare but dangerous condition caused by too much serotonin in the brain. Symptoms include high fever, rapid heartbeat, muscle rigidity, confusion, and seizures. It sounds terrifying. And for a while, doctors and patients believed it. The problem? The FDA didn’t have any real cases to back it up. They based the warning on theoretical pharmacology: both drugs affect serotonin, so maybe together they’re dangerous. That’s like saying two people holding water bottles might flood a room - ignoring that one bottle is just a sippy cup and the other is a hose. Triptans don’t increase serotonin levels. They don’t block reuptake. They don’t flood the system. They’re like specialized keys that only fit one lock: the 5-HT1B and 5-HT1D receptors in brain blood vessels. That’s how they stop migraines - by narrowing swollen vessels and blocking pain signals. They barely touch the 5-HT1A receptor, and they ignore the 5-HT2A receptor entirely. And here’s the critical part: serotonin syndrome isn’t caused by 5-HT1B or 5-HT1D activation. It’s caused by overstimulation of 5-HT2A receptors. That’s the receptor targeted by drugs like MDMA, certain antidepressants (especially nefazodone), and MAOIs. SSRIs increase serotonin overall - and yes, in overdose, they can trigger serotonin syndrome. But triptans? They’re not adding fuel to the fire. They’re just turning on a specific light switch.The Evidence That Changed Everything
In 2019, researchers from the University of Washington analyzed data from over 61,000 patients treated between 1990 and 2018. Every single one of them was taking both a triptan and an SSRI or SNRI. None developed serotonin syndrome that met strict diagnostic criteria. Zero. Not one. That study, published in JAMA Neurology, didn’t just challenge the FDA warning - it buried it. Other studies confirmed it. A 2010 review in Headache journal by Dr. P. Ken Gillman concluded there was “neither significant clinical evidence, nor theoretical reason, to entertain speculation about serious serotonin syndrome from triptans and SSRIs.” Even the FDA’s own adverse event database tells the story. From 2006 to 2022, there were only 18 reported cases where triptans and SSRIs were both involved. Experts reviewed them. None were confirmed as true serotonin syndrome. Most were misdiagnosed migraines, infections, or drug overdoses involving other substances. Meanwhile, serotonin syndrome from SSRIs alone? That’s real - but still rare. Studies show about 0.5 to 0.9 cases per 1,000 patient-months with certain SSRIs like nefazodone. And in overdose, about 14% of patients develop symptoms. But when you add a triptan? Nothing changes.
Why the Warning Still Exists
If the science is clear, why are pharmacists still blocking prescriptions? Because software doesn’t think. Pharmacy systems are programmed with alerts based on outdated FDA warnings from 2006. They don’t know about the 2019 JAMA study. They don’t know about receptor specificity. They just see “SSRI + Triptan” and flash a red warning. Many doctors, especially outside headache clinics, still believe the myth. Some patients have been denied triptans for years - even though they’ve been taking both safely for a decade. A 2022 survey by the American Migraine Foundation found 42% of 1,200 respondents were refused triptans because they took an antidepressant. Not because they had symptoms. Not because they’d ever had a problem. Just because of a computer alert. Even UpToDate, a trusted clinical reference, updated its entry in July 2023 to say the risk is “negligible.” But some older textbooks and online resources still list it as a “possible” interaction. That confusion costs patients time, money, and relief.What Doctors Are Actually Doing
In real-world practice, the tide has turned. A 2021 survey of 250 headache specialists found 89% routinely prescribe triptans with SSRIs or SNRIs without any special monitoring. The American Headache Society’s 2022 consensus statement says: “Clinicians should not avoid prescribing triptans to patients taking SSRIs or SNRIs due to theoretical concerns.” The European Medicines Agency never issued the warning. Why? Because they looked at the data - and saw nothing. Meanwhile, in the U.S., prescriptions for triptans alongside SSRIs have actually gone up - from 18.7% in 2007 to 32.4% in 2022. Patients and doctors are catching on. Pharmaceutical companies are quietly updating labels. The 2023 prescribing information for Imitrex (sumatriptan) still mentions the FDA warning - but adds: “Epidemiological studies have not shown an increased risk of serotonin syndrome with concomitant use of triptans and SSRIs/SNRIs.”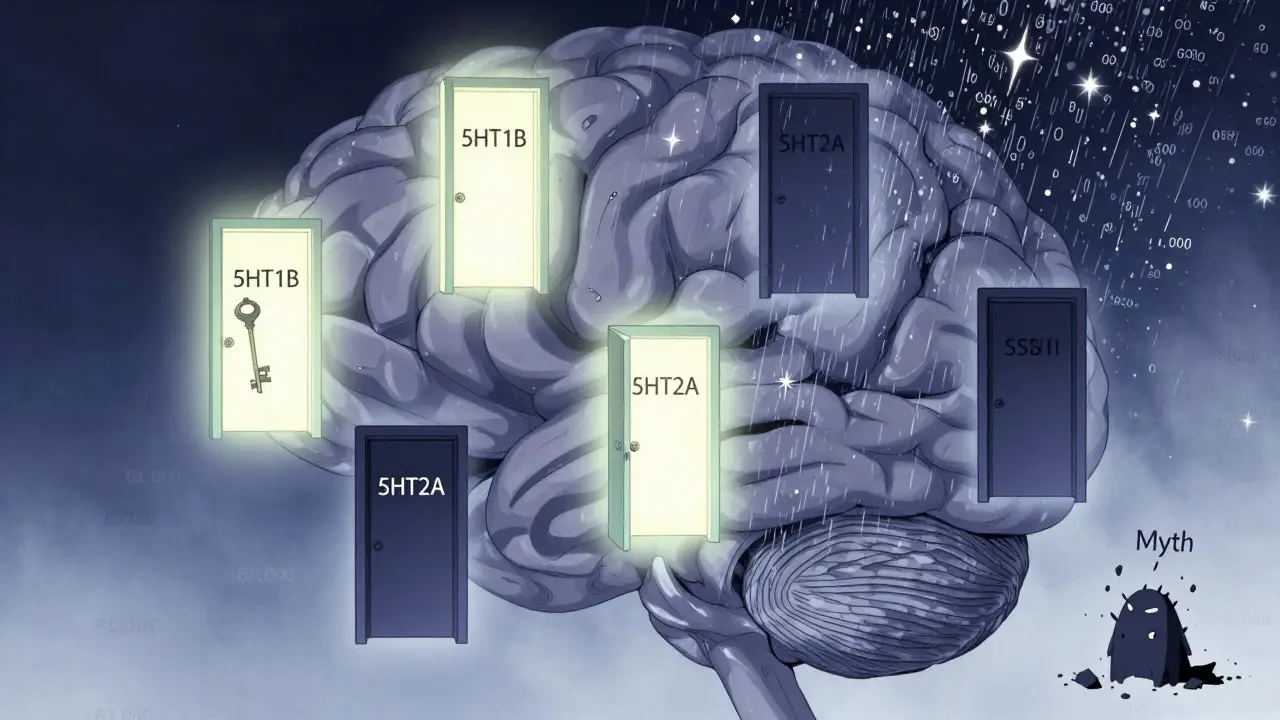
What This Means for You
If you take an SSRI or SNRI for depression, anxiety, or OCD - and you get migraines - you are not at risk from combining them with a triptan. You can safely use sumatriptan, rizatriptan, eletriptan, or any other triptan when you need it. There’s no need to space doses. No need to monitor for symptoms. No need to avoid the combination. If you’ve been told otherwise, you’ve been misled. The only time serotonin syndrome becomes a real concern is when you’re on multiple serotonergic drugs - like an SSRI plus an MAOI, or an SSRI plus tramadol or dextromethorphan in high doses. Those combinations are dangerous. Triptans? Not even close.What’s Next?
The American Headache Society and National Headache Foundation formally petitioned the FDA in 2023 to remove the warning. Their request is backed by 17 years of clinical data, zero confirmed cases, and overwhelming expert consensus. Meanwhile, researchers at Albert Einstein College of Medicine are tracking 10,000 patients on triptan-SSRI combinations. So far, through 2023, not one has developed serotonin syndrome. The Mayo Clinic’s 2023 position says it best: “The theoretical risk has not materialized in clinical practice.” This isn’t just about migraine treatment. It’s about trust in medicine. It’s about how warnings get created - and how slowly they get corrected. It’s about patients being denied effective care because of outdated alerts. You deserve better. You deserve to treat your migraines without fear. And now, you know the truth: triptans and SSRIs are safe together. The risk isn’t real. The fear was.Can I take a triptan if I’m on an SSRI?
Yes. There is no meaningful risk of serotonin syndrome from combining triptans with SSRIs or SNRIs. Major studies involving tens of thousands of patients have found zero confirmed cases. Leading medical societies now recommend this combination without restrictions.
Why do pharmacies still warn me about this?
Pharmacy software often still uses the outdated 2006 FDA warning as a trigger. These systems aren’t programmed to update based on new research. They see two serotonin-related drugs and flag them - even when the science says it’s safe. You may need to ask your doctor to override the alert or provide a letter explaining the evidence.
What’s the difference between serotonin syndrome and a migraine?
Migraines cause throbbing head pain, nausea, light sensitivity, and sometimes aura. Serotonin syndrome includes high fever, muscle rigidity, rapid heart rate, confusion, tremors, and hyperreflexia - symptoms that come on suddenly and are not typical of migraine. If you’re unsure, seek medical help. But remember: triptans don’t cause serotonin syndrome, even when combined with SSRIs.
Are there any antidepressants I should avoid with triptans?
Avoid combining triptans with MAOIs (like phenelzine or tranylcypromine), as that combination can cause serotonin syndrome. Also be cautious with high-dose tramadol, dextromethorphan, or certain illicit drugs like MDMA. SSRIs and SNRIs - including fluoxetine, sertraline, venlafaxine, and escitalopram - are safe with triptans.
Should I stop my SSRI before taking a triptan?
No. Stopping your SSRI unnecessarily can worsen depression or anxiety and may trigger rebound migraines. There is no medical reason to discontinue an SSRI to use a triptan. The combination is safe and commonly used by neurologists worldwide.
Is serotonin syndrome common with SSRIs alone?
It’s rare. Studies estimate 0.5 to 0.9 cases per 1,000 patient-months for certain SSRIs, and about 14% of patients with SSRI overdose develop symptoms. But adding a triptan doesn’t increase that risk. The danger comes from combining SSRIs with drugs that strongly increase serotonin levels - not from triptans.

10 Comments
Adrienne DaggDecember 18, 2025 AT 20:50
OMG I CAN’T BELIEVE THIS WASN’T COMMON KNOWLEDGE 😭 I’ve been denied triptans for 5 years bc of this stupid alert. My neurologist finally said ‘just ignore the pharmacy’ and I cried. Thank you for putting this out here.Erica VestDecember 20, 2025 AT 02:46
The 2019 JAMA Neurology study analyzed 61,000 patients with concurrent triptan and SSRI/SNRI use and found zero confirmed cases of serotonin syndrome. This is not anecdotal-it is statistically robust, peer-reviewed, and corroborated by multiple meta-analyses. The FDA’s 2006 alert was a theoretical overreaction based on pharmacokinetic speculation, not clinical evidence.Chris DavidsonDecember 20, 2025 AT 16:59
Pharmacies are still blocking prescriptions because they follow software rules not science. Doctors dont update their knowledge either. Patients suffer because systems dont evolve. Simple as thatKelly MulderDecember 20, 2025 AT 21:54
I find it profoundly concerning that the medical establishment continues to perpetuate a myth rooted in 2006-era pharmacological ignorance. The fact that UpToDate updated its guidance in 2023 while textbooks and pharmacy algorithms lag behind speaks to a systemic failure in knowledge dissemination. One might even say this is a case of institutional epistemic stagnation-where bureaucratic inertia overrides empirical truth.Tim GoodfellowDecember 20, 2025 AT 23:42
This is the kind of post that makes you want to high-five a stranger on the street 🙌 I’ve been on sertraline for 8 years and triptans for 6-never had a hiccup. The fact that people are still being denied relief because of a computer beep? That’s not just frustrating-it’s cruel. We need to riot. Or at least send angry emails to pharmacy chains.mark shortusDecember 22, 2025 AT 20:49
I JUST GOT DENIED A TRIPTAN YESTERDAY. I WAS SO ANGRY I CRIED IN THE PHARMACY. I’VE BEEN ON CITALOPRAM FOR 7 YEARS. I’VE TAKEN SUMATRIPTAN OVER 200 TIMES. I’M ALIVE. I’M OKAY. WHY IS THIS STILL A THING??? I FEEL LIKE I’M BEING TREATED LIKE A LAB RAT IN A 2006 TIME CAPSULE.Elaine DouglassDecember 24, 2025 AT 13:31
This means so much to me. I’ve been afraid to take my triptans for years because I didn’t want to risk something bad happening. I didn’t know the science. Thank you for explaining it so clearly. I’m going to talk to my doctor tomorrow.Takeysha TurnquestDecember 24, 2025 AT 21:58
The fear was never real. The fear was a mirror. It reflected our collective anxiety about control. About the fragility of the body. About trusting science when it contradicts authority. We clung to the warning not because it was true-but because it made us feel safe in our ignorance. The truth doesn’t comfort. It liberates.Emily PDecember 26, 2025 AT 13:41
Is there a public database where I can see the 18 reported cases the FDA mentioned? Just curious what they actually looked like.Jedidiah MasseyDecember 27, 2025 AT 07:51
The 5-HT1B/1D agonism profile of triptans is functionally orthogonal to the 5-HT2A hyperstimulation paradigm that underlies serotonin syndrome. Ergo, the pharmacodynamic overlap is negligible. The FDA’s 2006 advisory was a classic case of overinterpretation of in vitro data extrapolated to in vivo outcomes without clinical validation. The 2019 JAMA study is definitive. Any lingering caution is not evidence-based-it’s algorithmic dogma.