If you have psoriasis and were recently prescribed a beta-blocker for high blood pressure or heart issues, your skin flare-up might not be random. It could be the medication itself. While beta-blockers save lives by lowering heart rate and blood pressure, they’re also one of the most common drug classes linked to worsening psoriasis - sometimes even triggering it in people who never had it before.
How Beta-Blockers Can Trigger Psoriasis Flares
Beta-blockers like metoprolol, propranolol, and atenolol work by blocking adrenaline from binding to beta receptors in your heart and blood vessels. That’s good for your cardiovascular system. But those same receptors are also found in your skin. When beta-blockers interfere with them, it messes with the balance of immune cells and skin cell growth. This can cause keratinocytes - the main skin cells - to multiply too fast, leading to the thick, scaly patches typical of psoriasis.
The exact mechanism isn’t fully understood, but research points to a drop in cyclic AMP (cAMP), a molecule that helps regulate skin cell turnover and inflammation. Lower cAMP means more inflammation and faster skin cell production. Topical beta-blockers like timolol eye drops for glaucoma can even cause psoriasis flares through absorption into the bloodstream, showing how deeply these drugs can affect the skin.
Which Beta-Blockers Are Most Likely to Cause Problems?
Not all beta-blockers are created equal when it comes to skin risk. The ones most often tied to psoriasis flares include:
- Metoprolol (Lopressor, Toprol-XL)
- Propranolol (Inderal)
- Atenolol (Tenormin)
- Bisoprolol
- Pindolol (Visken)
- Timolol (eye drops for glaucoma)
Metoprolol is the most commonly prescribed beta-blocker in the U.S., with over 63 million prescriptions filled in 2023 alone. That means a lot of people with psoriasis are being exposed to this risk. Even though some beta-blockers are labeled as “cardioselective” (meaning they’re supposed to target the heart only), they still affect the skin enough to trigger flares in susceptible people.
How Long Does It Take for a Flare to Show Up?
One of the hardest parts about linking beta-blockers to psoriasis is the delay. You might start the medication and feel fine for months - even up to 18 months. Then, out of nowhere, your skin starts flaring. That’s why many patients don’t connect the dots until their dermatologist asks the right question.
One Reddit user, u/PsoriasisWarrior2024, shared that after six months on metoprolol, their psoriasis went from covering 5% of their body to 30%. They thought it was stress or diet - until they stopped the drug and saw improvement. That kind of story is common on patient forums like MyPsoriasisTeam, where people repeatedly report flares after starting beta-blockers.
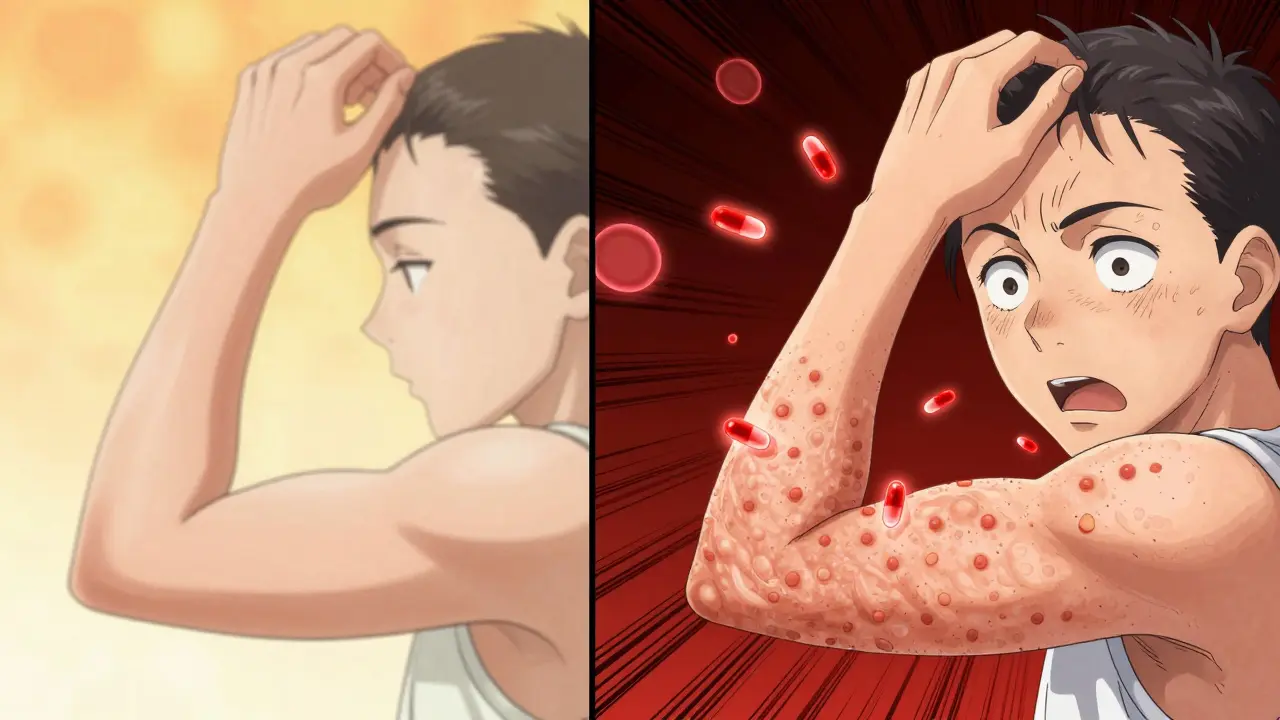
It’s Not Just Worsening - It Can Start Psoriasis Too
Most people assume beta-blockers only make existing psoriasis worse. But they can also cause psoriasis to appear for the first time. A 2010 study in the Journal of the American Academy of Dermatology found that beta-blockers were a major trigger for new-onset psoriasis in patients with no prior history. Even more telling: Practolol, an older beta-blocker, was pulled off the market in the 1980s because of its high rate of skin reactions, including psoriasiform eruptions.
That doesn’t mean every person on beta-blockers will get psoriasis. But if you’re genetically predisposed - especially if you carry the HLA-C*06:02 gene variant - your risk goes up. A 2024 study at Johns Hopkins and Mayo Clinic is currently testing whether this gene can predict who’s most likely to react. Early results suggest it might.
What Does the Evidence Really Say?
There’s conflicting data. One 2010 study (PMC2921739) said cumulative exposure to beta-blockers isn’t a major risk factor. But other research, including a 2022 update from DermNet NZ, says about 20% of people with psoriasis see their condition worsen after starting these drugs. A 2023 survey by MedicalNewsToday found that 37% of psoriasis patients on beta-blockers reported worsening symptoms - compared to just 12% of those on other blood pressure meds.
Here’s the key: clinical improvement after stopping the drug is the strongest indicator that the beta-blocker was the cause. If your skin clears up within weeks of discontinuing the medication, it’s likely the culprit.
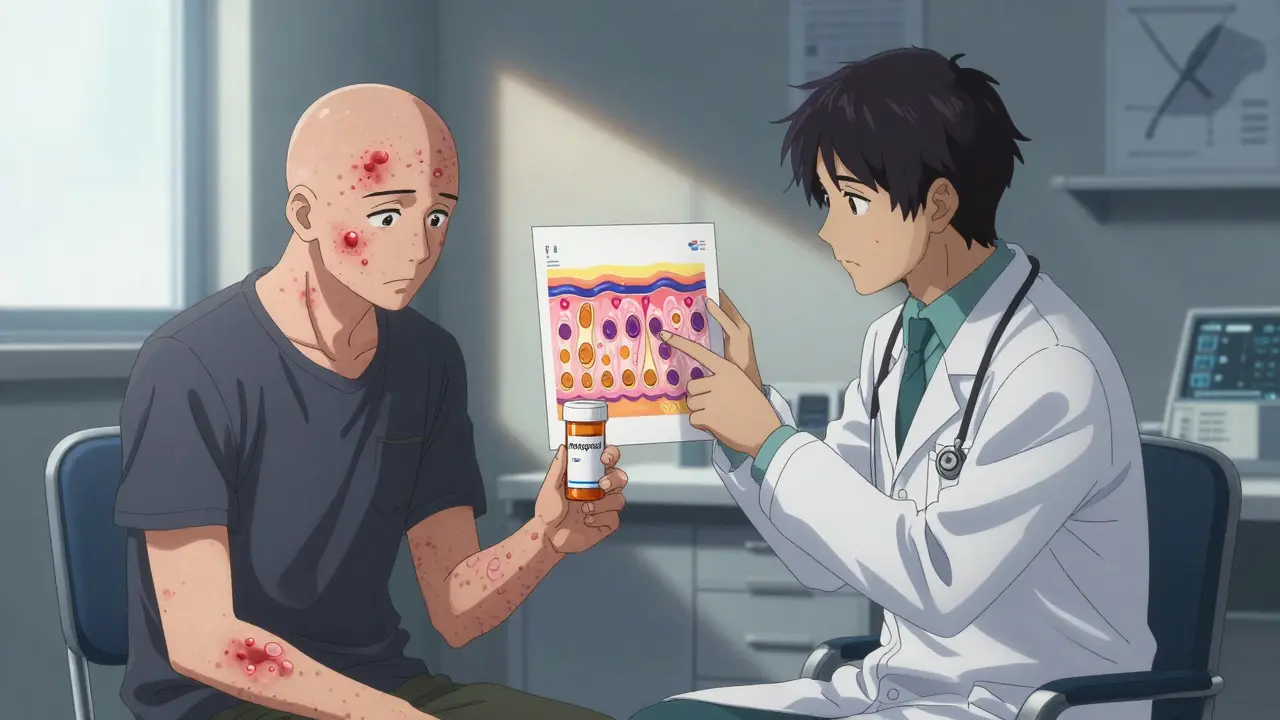
What Should You Do If You Suspect Your Medication Is Causing Flares?
Don’t stop your beta-blocker on your own. These drugs are often critical for preventing heart attacks, strokes, or dangerous heart rhythms. Instead:
- Track your symptoms. Note when your flare started and how it changed over time.
- Talk to your dermatologist and cardiologist together. They need to weigh your heart risks against your skin health.
- Ask if switching to another type of blood pressure medication is possible.
Good alternatives include:
- Calcium channel blockers like amlodipine
- ARBs like losartan
Be aware: ACE inhibitors (like lisinopril) can also trigger psoriasis in some people, so they’re not always a safe swap. Your doctors will pick the option that protects your heart without wrecking your skin.

How Is Beta-Blocker-Induced Psoriasis Treated?
If you’re diagnosed with medication-triggered psoriasis, treatment follows the same path as regular psoriasis - but with one big difference: stopping the beta-blocker is often the most effective step.
Once the drug is out of your system, doctors may use:
- Topical corticosteroids to reduce inflammation
- Vitamin D analogues like calcipotriene to slow skin cell growth
- Phototherapy (UV light treatment) for moderate to severe cases
- Systemic drugs like methotrexate or biologics if flares are widespread
Many patients see significant improvement within 4-8 weeks of stopping the beta-blocker, especially if they’re not on multiple triggering medications.
Real Stories, Real Impact
On MyPsoriasisTeam, a member wrote: “I was on metoprolol for 14 months. My scalp and elbows were covered. I thought I was just getting older. Then I stopped the drug - and within a month, my skin cleared by 70%.” Another user said, “My dermatologist didn’t even ask about my meds. I had to bring it up.”
That’s the problem. Many doctors don’t routinely ask about skin changes when prescribing heart meds. And patients don’t know to connect the two. If you have psoriasis and are on a beta-blocker, speak up. Bring this article to your next appointment. Ask: “Could this medication be making my skin worse?”
What’s Next?
Researchers are working on new beta-blockers that target only heart receptors and avoid skin ones. Some companies are testing topical formulations with minimal absorption. In the future, genetic testing might tell you if you’re at high risk before you even start the drug.
For now, awareness is your best tool. If you’re on a beta-blocker and your psoriasis has gotten worse - especially after months of stability - don’t ignore it. Your skin is sending a signal. Listen to it. Talk to your doctors. There are alternatives. And your skin deserves better than a guesswork approach.
Can beta-blockers cause psoriasis in someone who never had it before?
Yes. While beta-blockers are more commonly linked to worsening existing psoriasis, they can also trigger new-onset psoriasis in people with no prior history. Studies and case reports show that drugs like metoprolol, propranolol, and atenolol have caused psoriasiform eruptions in individuals who had never experienced psoriasis before starting these medications.
How long after starting a beta-blocker might psoriasis appear?
The timeline varies widely. Some people notice skin changes within a few weeks, while others may not see a flare until 6 to 18 months after starting the medication. This delayed onset makes it hard to link the drug to the symptom without careful tracking and medical guidance.
Are all beta-blockers equally likely to trigger psoriasis?
No. Propranolol, metoprolol, atenolol, bisoprolol, and pindolol are most frequently linked to psoriasis flares. Even “cardioselective” beta-blockers like metoprolol can still affect the skin. Topical forms like timolol eye drops can also cause flares through systemic absorption. Not everyone reacts the same way, but if one beta-blocker triggers a flare, others likely will too.
What should I do if I think my beta-blocker is making my psoriasis worse?
Do not stop taking the medication without talking to your doctor. Contact both your dermatologist and cardiologist to discuss your symptoms. They can evaluate whether switching to a different class of blood pressure medication - like a calcium channel blocker or ARB - is safe and appropriate for your heart health.
Is there a genetic test to predict if I’ll react to beta-blockers?
Not yet for routine use, but research is underway. A 2024 study at Johns Hopkins and Mayo Clinic is investigating whether people with the HLA-C*06:02 gene variant - already linked to psoriasis susceptibility - are more likely to develop flares from beta-blockers. Early results suggest this gene may help identify high-risk patients before they start the medication.
Can I use topical corticosteroids if my psoriasis is caused by beta-blockers?
Yes. Topical corticosteroids, vitamin D analogues, and phototherapy are standard treatments for beta-blocker-induced psoriasis. However, these manage the symptoms - they don’t fix the root cause. The most effective long-term solution is usually switching the triggering medication, especially if the flare improves after stopping the beta-blocker.
Are there any blood pressure medications that are safer for people with psoriasis?
Calcium channel blockers like amlodipine and ARBs like losartan are generally considered safer alternatives for people with psoriasis. ACE inhibitors may also trigger flares in some cases, so they’re not always a better option. Your doctor will choose the best alternative based on your heart condition and overall health.

8 Comments
Austin Mac-AnabrabaJanuary 2, 2026 AT 03:59
Let’s be clear: this isn’t ‘medication side effect’-it’s pharmaceutical negligence masked as science. Beta-blockers were never designed with skin biology in mind, yet they’re shoved into millions of prescriptions like they’re aspirin. The fact that we’re still debating whether metoprolol triggers psoriasis in 2024 is a failure of medical epistemology. We have the molecular pathways mapped, the clinical correlations documented, and yet the standard of care remains ‘wait and see’ until your skin looks like a reptile shed. That’s not medicine. That’s procedural inertia.
Phoebe McKenzieJanuary 3, 2026 AT 06:20
Ugh. I knew someone would post this. My cousin was on propranolol for 3 years and her psoriasis went from ‘mild scalp’ to ‘full-body armor.’ Her cardiologist told her to ‘use more moisturizer.’ I swear to god, if doctors treated heart disease like they treat skin like a cosmetic issue, people would be dropping dead in waiting rooms. STOP MINIMIZING THIS. It’s not ‘a flare’-it’s your immune system screaming because your meds are poisoning your skin. And yes, it’s the drug. Not stress. Not diet. Not your ‘weak immune system.’ It’s the damn beta-blocker.
gerard najeraJanuary 4, 2026 AT 21:36
Stop the drug. Watch the skin heal. That’s the diagnostic test.
Donna PeplinskieJanuary 5, 2026 AT 18:24
Thank you for writing this-seriously. I’ve been living with psoriasis for 12 years, and when I started atenolol last year, I thought I was just ‘getting older.’ I didn’t connect it until I read someone else’s story online. I told my doctor, and we switched me to losartan. My elbows? Barely red now. My scalp? Back to normal. It took six weeks, but it happened. I just wish my dermatologist had asked about my meds sooner. Please, if you’re on any beta-blocker and your skin’s acting up… don’t assume it’s ‘just psoriasis.’ Ask. Advocate. You’re not overreacting. Your body’s giving you data.
Liam GeorgeJanuary 6, 2026 AT 02:55
Did you know that Big Pharma funded the 2010 study that said ‘no major risk’? The same companies that make beta-blockers also own the dermatology journals. The HLA-C*06:02 gene? They’ve known about it since 2007. Why isn’t it in the prescribing info? Why aren’t we getting genetic screening before these prescriptions? This isn’t an accident. It’s a profit-driven cover-up. They’d rather have you on biologics for $100K/year than switch you to a $2 calcium channel blocker. And don’t get me started on timolol eye drops-those are literally dripping into your bloodstream. They don’t warn you because they don’t want you to know.
sharad vyasJanuary 7, 2026 AT 06:12
India has been using beta-blockers for decades and psoriasis rates are way lower here. Maybe it's not the drug? Maybe it's the diet? Or the stress? Or maybe western medicine just loves to blame pills for everything. I've seen people with psoriasis here on metoprolol-no problem. It's not the drug. It's the lifestyle.
Dusty WeeksJanuary 7, 2026 AT 20:54
bro i was on metoprolol for 8 months and my elbows looked like cracked leather 😭 i thought i was dying. i stopped it cold turkey (bad idea, i know) and my skin cleared in 3 weeks. my doc was like ‘huh, weird’ 🤷♂️ now i’m on amlodipine and my skin is chill. if you’re on beta-blockers and your skin is mad… try stopping it. just for a bit. your skin will thank you. 🙏💊
Sally Denham-VaughanJanuary 9, 2026 AT 12:45
Thank you, thank you, THANK YOU for this. I’m a nurse and I’ve seen this exact thing happen three times this year alone. Patients come in with ‘new’ psoriasis, and we don’t even think to ask about meds. I started asking after my own mom’s flare-up after starting bisoprolol. Now I always ask: ‘What are you on?’ And if they’re on a beta-blocker? I say, ‘Let’s talk to your cardiologist about switching.’ It’s not hard. It’s not complicated. It’s just not taught. We need to change that. Your skin matters too.