Pheochromocytoma Management: A Practical Guide
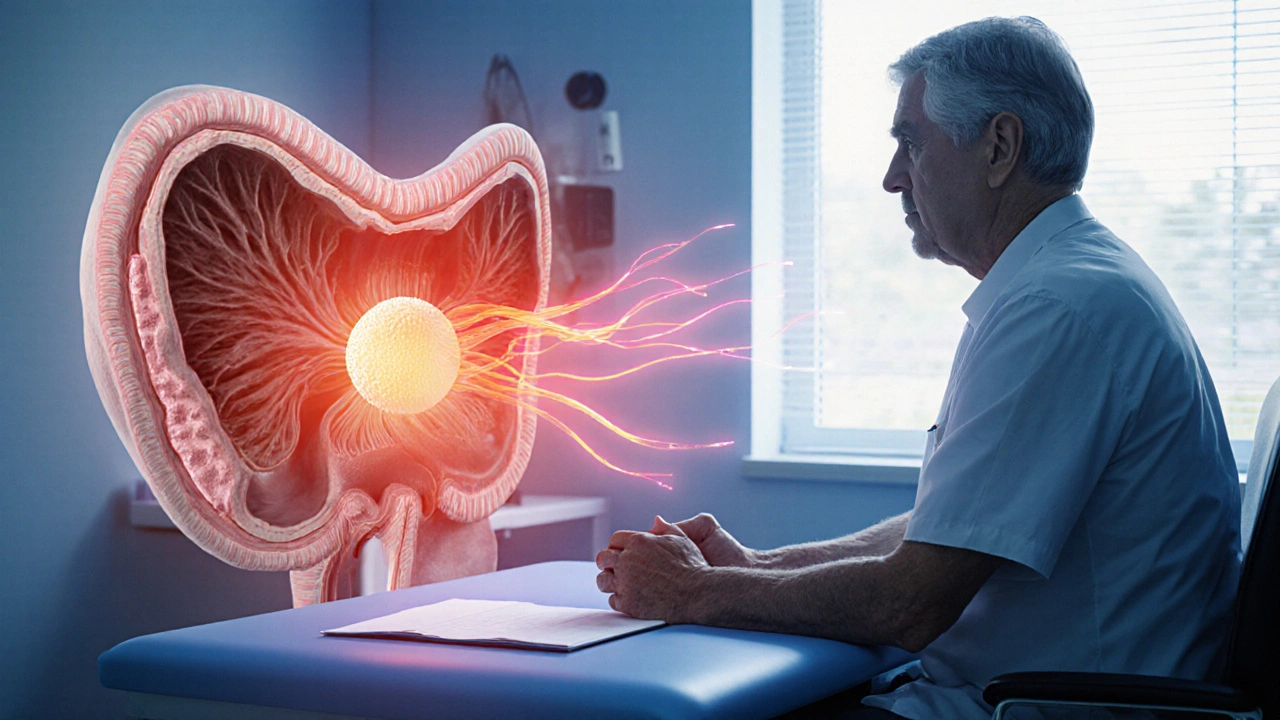
When dealing with pheochromocytoma, a rare catecholamine‑producing tumor of the adrenal medulla. Also known as adrenal pheochromocytoma, it can cause sudden spikes in blood pressure, heart palpitations, and sweating. Proper pheochromocytoma management means controlling these symptoms, removing the tumor safely, and preventing recurrence.
The first pillar of care is accurate diagnosis. Lab tests measuring plasma free metanephrines or urinary fractionated catecholamines confirm excess hormone production. Imaging—CT, MRI, or functional scans such as 123I‑MIBG—pinpoints the tumor’s location and size. Early detection is critical because untreated pheochromocytoma can trigger life‑threatening hypertensive crises.
Key Steps in Effective Management
Once the tumor is identified, Alpha‑blockade, the use of medications that block alpha‑adrenergic receptors to control blood pressure before surgery becomes the next essential step. Drugs like phenoxybenzamine or selective agents such as doxazosin tame the surge of catecholamines, allowing patients to reach a stable hemodynamic baseline. This pre‑operative preparation reduces intra‑operative spikes and improves surgical outcomes.
After adequate alpha‑blockade, the definitive treatment is Surgical resection, removing the pheochromocytoma via laparoscopic or open adrenalectomy. Laparoscopic approaches dominate for small, localized tumors, offering quicker recovery and less pain. Open surgery remains the choice for large or invasive tumors. The surgeon must coordinate closely with anesthesiologists familiar with catecholamine‑induced hemodynamic swings.
Genetics play a bigger role than many realize. Up to 40% of patients have a hereditary predisposition, so Genetic testing, screening for mutations in genes like RET, VHL, NF1, and SDHx that increase tumor risk is recommended for all confirmed cases. Identifying a mutation guides family screening, informs surveillance intervals, and can influence surgical planning if multiple lesions are likely.
Follow‑up completes the management cycle. Regular biochemical testing (every 6‑12 months) and imaging when indicated catch recurrent or metastatic disease early. Patients also need education about symptom awareness—sudden headaches, palpitations, or sweating could signal tumor activity. Lifestyle tweaks, such as stress reduction and avoiding catecholamine‑triggering substances, support long‑term stability.
All these components—diagnosis, alpha‑blockade, surgery, genetics, and vigilant follow‑up—interlock to form a comprehensive approach. Below you’ll find articles that dive deeper into each area, offering step‑by‑step guides, medication comparisons, and real‑world tips you can apply right away.
Practical advice for living with pheochromocytoma, covering symptoms, medication, diet, exercise, emergency plans, and mental health tips.