Penicillin Desensitization: What It Is and When It’s Needed
When someone has a true penicillin desensitization, a medical process that temporarily allows a person with a penicillin allergy to take the drug safely. Also known as allergy induction therapy, it’s not a cure—but it’s the only way many patients can use penicillin when it’s the best or only effective antibiotic for their infection. About 10% of people say they’re allergic to penicillin, but less than 1% actually have a true IgE-mediated allergy. Most people outgrow it, misremember a childhood rash, or confuse side effects like nausea with an allergy. But for those who do have a confirmed severe reaction—like anaphylaxis, hives, or swelling—avoiding penicillin can mean using less effective, more toxic, or more expensive drugs.
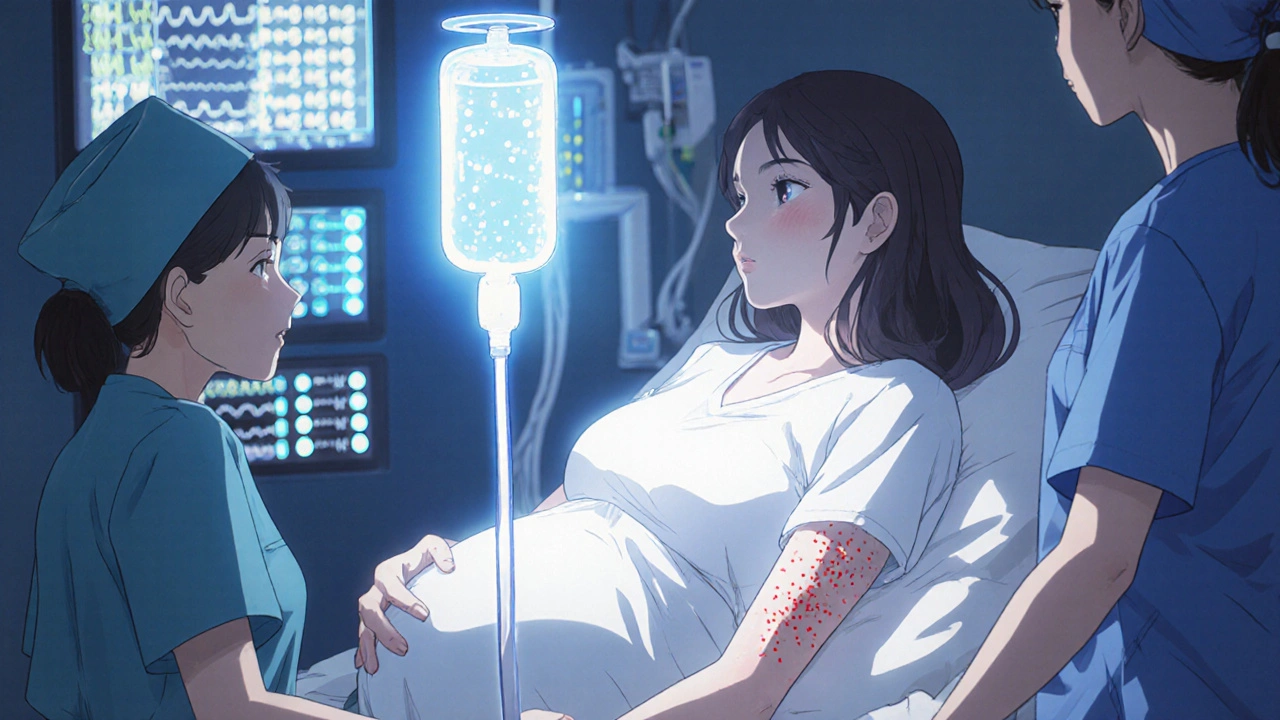
That’s where penicillin allergy, a potentially life-threatening immune response triggered by penicillin or related antibiotics becomes a clinical problem. If you have pneumonia, endocarditis, or syphilis, and penicillin is the gold-standard treatment, skipping it can cost you your health. That’s why hospitals run drug desensitization, a controlled process of gradually increasing doses of an allergenic drug under medical supervision in controlled settings. It’s not done lightly. You need a clear diagnosis, a trained team, and a reason why no other antibiotic will work. The process usually takes 6 to 12 hours. You get tiny, increasing doses of penicillin—every 15 to 30 minutes—while being watched for signs of reaction. If you react, they stop, treat you, and try again later. If you don’t, you’re then able to take full therapeutic doses safely—for that one course of treatment.
It’s not permanent. Once you stop taking penicillin for more than a few days, your body forgets the tolerance. So if you need it again next year, you’ll likely need to go through desensitization again. But for someone in critical condition—say, a pregnant woman with syphilis or a patient with a resistant staph infection—it’s the difference between life and death. This isn’t a home remedy. It’s not something you do with a pharmacist’s advice. It’s strictly hospital-based, with emergency equipment on standby.
What you’ll find in the posts below is a collection of real-world cases and clinical insights that tie into this topic. You’ll see how drug interactions, antibiotic resistance, and allergic reactions shape treatment choices. You’ll learn how medications like Bactroban and clindamycin are used when penicillin isn’t an option. You’ll see how repeated antibiotic use affects the body over time—and why knowing your true allergy status matters more than ever. This isn’t theory. It’s what doctors face every day when the safest drug is also the one your body says no to. And sometimes, the only way forward is to slowly, carefully, convince your immune system to let it in.
Penicillin desensitization safely allows allergic patients to receive life-saving penicillin when no alternatives exist. Learn how it works, who qualifies, and why it’s critical in fighting antibiotic resistance.