Healthcare Spending: What It Costs and Who Pays
When you hear healthcare spending, the total money spent on medical services, medications, and treatments across a population. Also known as medical expenditure, it’s not just about hospitals—it’s about whether your prescription gets covered, if a life-saving drug is available, or if you’re forced to choose between food and your meds. This isn’t abstract. It’s the reason some people skip doses because the co-pay is $200, and it’s why hospitals run out of antibiotics and have to decide who gets the last vial.
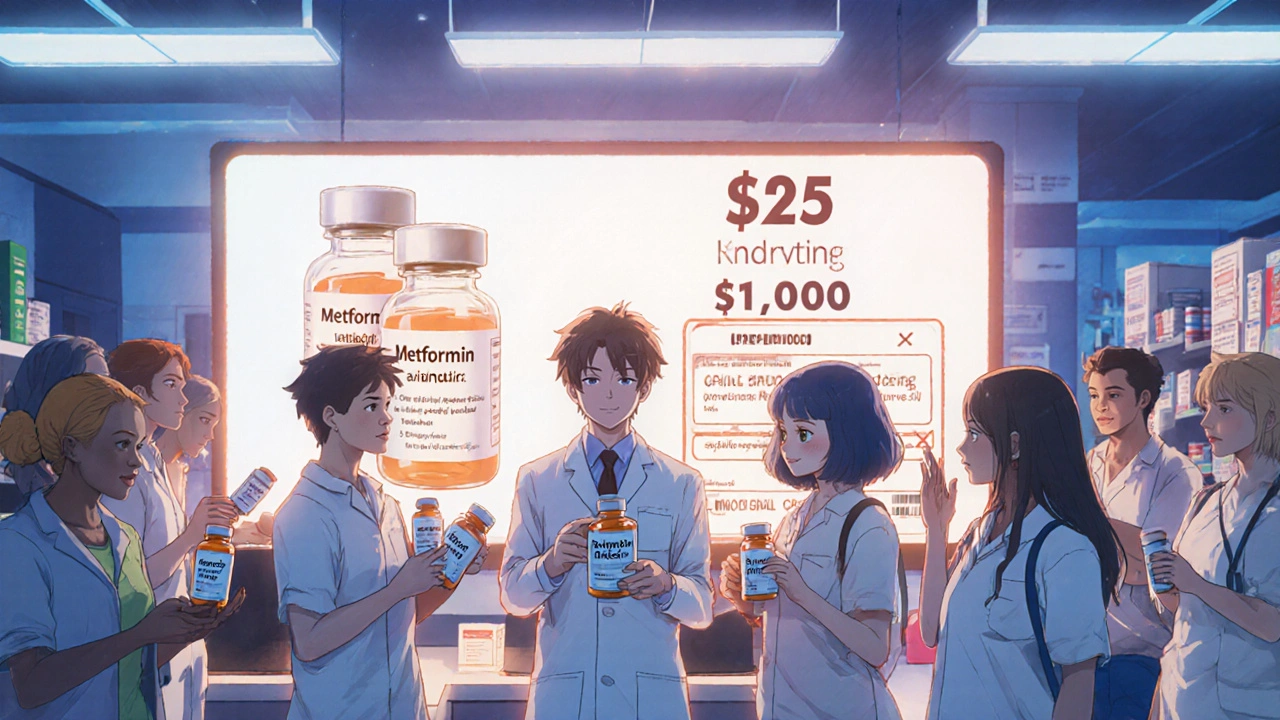
Drug pricing, how much pharmaceutical companies charge for medications, often with little transparency. Also known as pharmaceutical costs, it directly feeds into healthcare spending. A single course of an antibiotic can cost $500 in the U.S. but under $10 elsewhere. That gap isn’t about production—it’s about patents, marketing, and who gets to set the price. Meanwhile, generic drugs, which make up over 90% of prescriptions in the U.S., cut those costs by 80-95%. Yet even generics aren’t always affordable when insurance doesn’t cover them or when supply chains break down.
When drugs run short, healthcare ethics kicks in. Hospitals don’t just pick who gets treatment randomly—they use frameworks based on survival odds, urgency, and fairness. That’s not theory. It’s real policy, used during opioid shortages, cancer drug delays, and now with insulin. And it’s tied to medication costs because when a brand-name drug is too expensive, clinics turn to cheaper alternatives—even if they’re less studied. That’s why you’ll find posts here about penicillin desensitization, generic substitution in workers’ comp, and why acid-reducing pills can mess with other drugs. It’s all connected: cost affects access, access affects outcomes, and outcomes affect who lives and who doesn’t.
You won’t find fluff here. No vague claims about "improving care." Just real stories: how a $500 migraine pill gets replaced by a $3 generic, why a diabetic skips insulin because their deductible reset, how a hospital rationing list saves lives but breaks hearts, and how a $100 hearing aid becomes a luxury. These are the hidden costs behind every prescription, every emergency room visit, every decision made behind closed doors. What follows are posts that dig into those moments—the science, the policy, the human impact. You’ll see how drug interactions, supply chains, and insurance rules all tie back to one thing: who pays, and who pays the price.
Generics are the backbone of affordable global healthcare, saving trillions while 37 countries cut spending. Discover how low-cost drugs keep millions alive - and why they're under threat.