Genetic Differences in Drug Metabolism
When you take a pill, your body doesn’t treat it the same way everyone else does. That’s because of genetic differences in drug metabolism, variations in your DNA that change how quickly or slowly your body breaks down medications. Also known as pharmacogenetics, this is why two people on the same dose of the same drug can have totally different outcomes—one gets relief, the other gets sick. It’s not about how much you weigh, what you ate, or if you forgot to take it on time. It’s built into your genes.
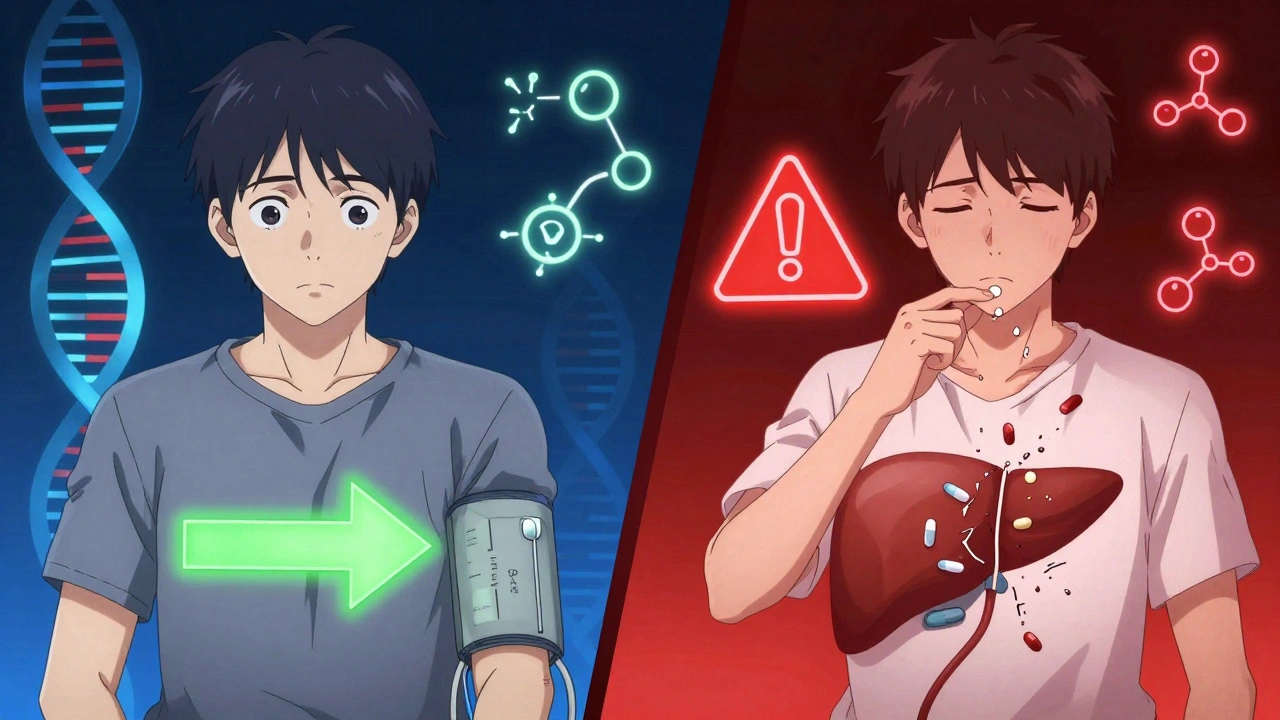
These differences mostly come from enzymes in your liver, especially the CYP450 enzymes, a family of proteins responsible for breaking down over 75% of all prescription drugs. Also known as cytochrome P450 system, these enzymes act like molecular scissors that chop up drugs so your body can flush them out. Some people have versions of these enzymes that work too fast—they clear the drug before it has time to help. Others have slow versions—the drug builds up and causes side effects. For example, if you’re a slow metabolizer of codeine, you might not get pain relief at all. If you’re a super-fast one, you could turn it into morphine too quickly and risk overdose. The same goes for antidepressants, blood thinners, and even statins.
These genetic quirks don’t just affect how drugs work—they affect which drugs you should even take. That’s why doctors are starting to use personalized medicine, tailoring treatments based on your genetic profile instead of using a one-size-fits-all approach. Also known as precision medicine, this isn’t science fiction—it’s already being used for cancer drugs, heart medications, and psychiatric treatments. If your liver can’t handle a certain drug, your doctor can switch you to one that doesn’t rely on the same enzyme. No trial and error. No dangerous side effects. Just smarter prescribing.
And it’s not just about what’s in your blood. Your genes also influence how your gut absorbs drugs, how your kidneys clear them, and even how your brain responds to them. That’s why a medication that works wonders for your neighbor might leave you dizzy or nauseous. It’s not you being difficult—it’s your biology.
What you’ll find below are real, practical articles that break down exactly how these genetic differences show up in everyday medicine. You’ll learn how liver disease changes drug processing, why grapefruit messes with statins, how antibiotics can mess with birth control, and why some people need completely different doses of the same pill. These aren’t theory pieces—they’re based on what doctors and pharmacists see every day. You’ll walk away knowing why your meds work (or don’t) and what to ask your doctor next time you’re prescribed something new.
Ethnicity influences how your body processes medications due to genetic differences in drug metabolism. Learn how CYP450 enzymes, HLA variants, and pharmacogenomics are changing prescribing practices to improve safety and effectiveness.