NMS Symptom Recognition & Risk Assessment Tool
NMS Symptom Recognition Tool
Identify potential NMS cases using the classic tetrad. Select symptoms to assess risk level. Time is critical in NMS diagnosis.
Muscle Rigidity
"Lead pipe" rigidity (stiff muscles that don't bend even with force)
High Fever
Fever above 103°F (39.4°C) that doesn't respond to acetaminophen
Altered Mental State
Confusion to mutism to coma
Autonomic Instability
Heart rate >120 bpm, blood pressure swings, sweating
Medication Risk Factors
Patient Risk Factors
Critical Next Steps
Important Information
Even one NMS symptom should prompt immediate medical attention. The article emphasizes that NMS is a medical emergency requiring immediate ICU care. Misdiagnosis occurs in up to 12% of cases, often mistaken for infection or worsening psychosis. Early recognition is critical for survival (95% survival rate with prompt treatment).
What Is Neuroleptic Malignant Syndrome?
Neuroleptic Malignant Syndrome is a rare but life-threatening reaction to medications that block dopamine in the brain, most commonly antipsychotics like haloperidol, risperidone, or olanzapine. It’s not an allergic reaction-it’s a neurological emergency caused by sudden, severe disruption of dopamine signaling. First identified in the 1950s after the introduction of chlorpromazine, it affects roughly 1 in every 1,000 people taking these drugs, though the risk drops significantly with newer medications. The condition doesn’t wait for warning signs. It hits fast, and if missed, it can kill.
The Four Signs You Can’t Ignore
There’s a clear pattern to NMS, and if you see even three of these, it’s time to act. The classic tetrad includes: muscle rigidity, high fever, changed mental state, and autonomic chaos. This isn’t just stiff muscles-it’s "lead pipe" rigidity, where limbs feel like they’re locked in concrete. You can’t bend the elbow, even with force. The fever isn’t a 101°F cold-this is 103°F or higher, often above 104°F, and it won’t break with acetaminophen. Mental status shifts from confusion to mutism to coma. Autonomic instability means your body loses control: heart racing at 120 beats per minute, blood pressure swinging wildly, sweating like you’re in a sauna despite cold skin.
These symptoms usually show up within the first two weeks of starting or increasing an antipsychotic. But they can also appear after stopping a dopamine drug like levodopa in Parkinson’s patients. One patient on Reddit described waking up unable to move or speak, with a temperature of 105.1°F. His doctors thought it was a psychotic break. It wasn’t. It was NMS.
Why This Happens: The Dopamine Breakdown
Antipsychotics work by blocking dopamine receptors-specifically D2 receptors-in the brain. That’s how they calm hallucinations and delusions. But dopamine isn’t just about thoughts. It’s also critical for movement, temperature control, and automatic body functions like heart rate and digestion. When those receptors in the hypothalamus and basal ganglia get blocked too hard or too fast, your body’s thermostat goes haywire, muscles lock up, and your autonomic nervous system spirals out of control. This isn’t a side effect you can ignore-it’s a system-wide failure.
Some medications outside antipsychotics can trigger this too. Anti-nausea drugs like metoclopramide and promethazine also block dopamine. That’s why NMS isn’t just a psychiatric issue. It can strike someone taking metoclopramide for reflux, or someone who just had surgery and got a shot of promethazine for vomiting.
How Doctors Diagnose It
There’s no single blood test for NMS. Diagnosis is clinical-based on symptoms, timing, and ruling out other causes. But labs help confirm it. Creatine kinase (CK) levels spike because muscle tissue is breaking down. Levels over 1,000 IU/L are common; in severe cases, they hit 100,000. That’s rhabdomyolysis-the same process that can happen after a crushing injury. Your muscles are literally dissolving.
Other signs: white blood cell count above 12,000, low iron (under 60 µg/dL), acid in the blood, low oxygen, and high potassium. Kidney damage follows fast-myoglobin from dead muscle clogs the kidneys. About 30% of NMS patients develop acute kidney injury. Liver enzymes rise too. These aren’t random numbers-they’re warning flags.
Doctors must rule out other conditions. Serotonin syndrome looks similar but comes on faster-within hours, not days. It causes clonus (involuntary muscle jerks), not lead-pipe rigidity. Malignant hyperthermia is even quicker, triggered by anesthesia, and often includes jaw spasms. NMS doesn’t have those. Misdiagnosis happens in up to 12% of cases. Too often, patients are treated for infection or worsening psychosis when they’re dying from NMS.
What Happens If You Don’t Act
Untreated NMS kills 10 to 20% of people. Even with treatment, 5% still die. The biggest killers are kidney failure, heart rhythm problems, and blood clots from immobility. The longer you wait, the worse it gets. Every hour without stopping the drug increases the risk of permanent muscle damage or brain injury. One patient spent eight weeks in rehab after NMS because his muscles were so damaged he couldn’t walk. He didn’t lose his life-but he lost months of his life.
Survival rates have improved from 76% in the 1980s to 95% today, not because of new miracle drugs, but because hospitals now recognize it faster. The key is speed. Stop the drug. Cool the body. Hydrate. Monitor. That’s it. No magic bullets.
How It’s Treated
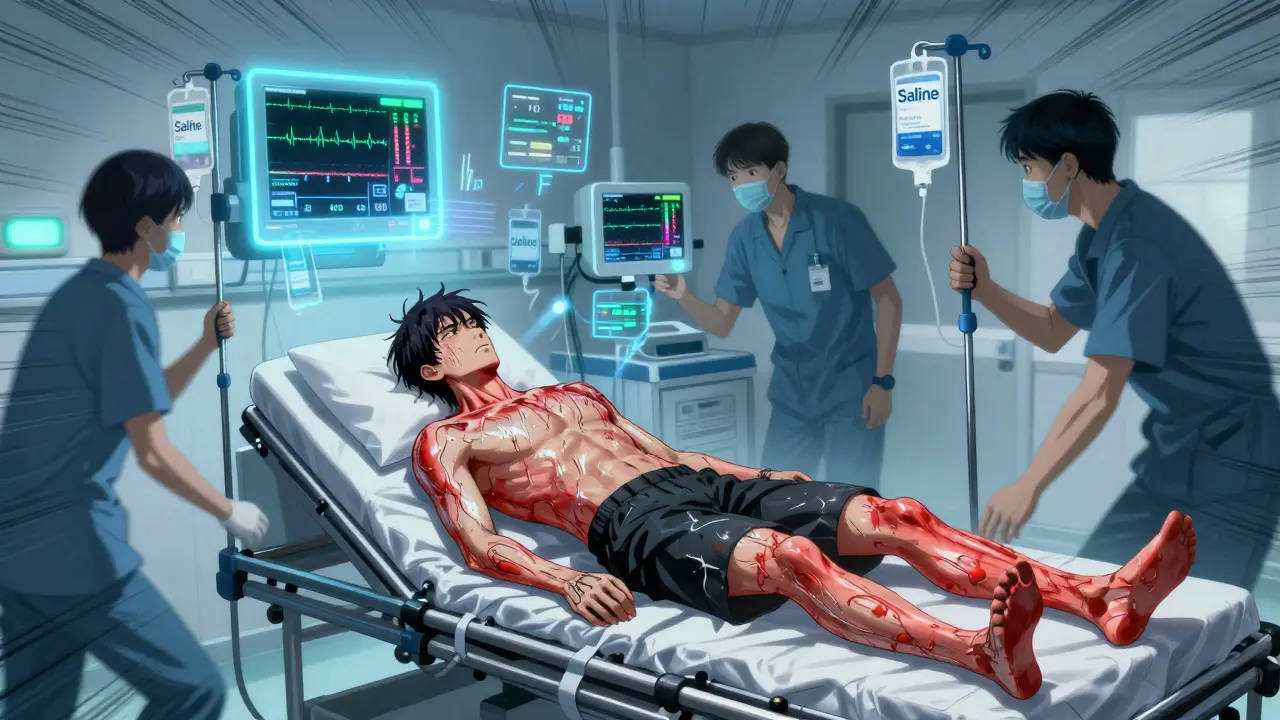
Step one: Stop everything. No more antipsychotics. No more metoclopramide. No exceptions. Step two: Get to the ICU. This isn’t a hospital ward case-it’s intensive care. Temperature control is critical. Ice packs, cooling blankets, IV fluids. Step three: Hydrate aggressively. Two liters of saline right away, then keep fluids going to flush out muscle debris and protect the kidneys. Urine output must stay above 30 mL per hour.
Medications help too. Dantrolene, a muscle relaxant used for malignant hyperthermia, is often given IV at 1-2.5 mg/kg and can be repeated. It doesn’t fix the dopamine problem, but it stops the muscles from tearing themselves apart. Bromocriptine, a dopamine agonist, is used to restart dopamine signaling. It’s given orally every 8 hours. Some hospitals are testing intranasal apomorphine-early results show it can lower fever in under four hours.
Monitoring is relentless. CK levels every 6-12 hours. Electrolytes. Kidney function. Oxygen. Heart rhythm. You can’t afford to miss a single shift. Recovery takes 7 to 10 days if caught early. But muscle weakness can linger for weeks. Some patients need physical therapy for months.
Who’s at Highest Risk?
It’s not random. Young men are more likely to develop NMS than women-about twice as often. People with mood disorders like bipolar disorder are at higher risk than those with schizophrenia. Rapid dose increases are the biggest trigger. Jumping haloperidol from 5mg to 15mg in one day? That’s a red flag. Parenteral (injected) forms of antipsychotics carry higher risk than pills. Mixing in lithium? Double the danger. And yes-it can happen even at "therapeutic" doses in people with no known risk factors. The FDA added a black box warning for this exact reason in January 2023.
Second-generation antipsychotics like quetiapine or aripiprazole are much safer. The risk dropped from 0.5-2% with older drugs like haloperidol to just 0.01-0.02% with newer ones. That’s why many doctors now start with these. But they’re not risk-free. NMS still happens.
What Happens After Recovery?
Survivors often face a terrifying choice: go back on antipsychotics or risk a psychotic relapse. A 2022 survey found 65% of NMS survivors were afraid to restart medication-even if they still heard voices or felt paranoid. That’s a huge problem. Many patients stop meds cold, leading to hospital readmissions. Some doctors wait weeks or months before reintroducing antipsychotics, starting with low-dose atypicals and monitoring closely. Others avoid them entirely, using non-dopamine-blocking treatments like mood stabilizers or psychotherapy.
There’s no perfect answer. But awareness is growing. Hospitals now train ER staff on NMS recognition. AI tools are being tested to flag risk factors in electronic records before symptoms even appear. One pilot system caught 85% of cases 24 hours before doctors noticed anything wrong.
What You Need to Know
If you’re on an antipsychotic-or caring for someone who is-know these signs: stiff muscles, high fever, confusion, and erratic heartbeat. Don’t assume it’s "just psychosis" or "a bug." Call 999 or go to A&E immediately. If you’ve had NMS before, tell every doctor you see. Keep a medical alert card. Don’t take metoclopramide unless you’ve told them about your history.
The good news? It’s rare. The better news? If caught early, you’ll likely survive. The best news? We’re getting better at spotting it before it’s too late. But only if we stop ignoring the signs.
Can Neuroleptic Malignant Syndrome happen with antidepressants?
No, not typically. Antidepressants like SSRIs or SNRIs don’t block dopamine receptors the way antipsychotics do. But they can cause serotonin syndrome, which has similar symptoms like fever and muscle rigidity-but it’s a different condition with different triggers and treatments. The key difference is clonus and hyperreflexia in serotonin syndrome, not lead-pipe rigidity.
Is NMS the same as malignant hyperthermia?
No. Malignant hyperthermia is triggered by anesthesia drugs like succinylcholine or halothane during surgery. It hits within minutes, causes jaw spasms, and is genetic. NMS develops over days, is caused by dopamine blockers, and affects people on long-term psychiatric meds. Both can be treated with dantrolene, but the triggers and timing are completely different.
Can you get NMS from stopping antipsychotics too fast?
Yes. While most cases happen when starting or increasing a drug, about 5% occur when dopamine medications like levodopa are suddenly stopped in Parkinson’s patients. Symptoms appear within 24 to 72 hours. That’s why tapering is critical-not just for psychiatric drugs, but for any dopamine-affecting medication.
How long does it take to recover from NMS?
With prompt treatment, most people start improving in 7 to 10 days. But full recovery can take weeks or months. Muscle weakness, fatigue, and cognitive fog are common for up to 30 days. About 15% of survivors still have noticeable muscle issues after a month. Recovery isn’t just about the fever breaking-it’s about rebuilding damaged tissue.
Are there any new treatments for NMS?
Yes. A phase II trial is testing intranasal apomorphine, which can lower fever in under four hours-much faster than traditional methods. AI tools are also being used to predict NMS before symptoms appear by analyzing EHR data. These aren’t standard yet, but they’re changing how hospitals respond. The goal is to catch it before it becomes an emergency.

9 Comments
Sami SahilFebruary 1, 2026 AT 05:23
bro this hit different. i had a cousin on risperidone and one day he just locked up like a robot, fever sky-high, no response. they thought it was a drug trip. turned out to be NMS. he spent 3 weeks in ICU. never thought meds could do that.franklin hillaryFebruary 2, 2026 AT 19:55
NMS is the silent killer no one talks about until it’s too late. i’ve seen it in the ER three times. every single time the family blamed the patient for being "too dramatic" or "just psychotic." the truth? their body was melting from the inside. stop calling it a mental health issue. it’s a neurochemical nuclear meltdown. dantrolene saves lives. know it. use it. spread it.Naomi WalshFebruary 3, 2026 AT 23:24
How quaint that you’re all acting like this is some groundbreaking revelation. The tetrad was described by Delay and Deniker in 1957. The CK elevation? Obvious. The dopamine hypothesis? Basic neuropharmacology. What’s truly concerning is that medical education still treats this as a rare curiosity rather than a core differential. If you’re not screening for NMS in every patient on antipsychotics with unexplained rigidity, you’re not just negligent-you’re dangerously unqualified.Melissa MelvilleFebruary 5, 2026 AT 06:38
OMG i had no idea metoclopramide could do this 😱 my grandma got that for nausea after surgery and almost died. why isn’t this on the bottle??Deep RankFebruary 6, 2026 AT 10:00
i mean like… i get why people are scared but honestly? if you’re on antipsychotics and you’re not getting regular blood work and a full neuro check every 2 weeks, you’re just asking for trouble. and dont even get me started on people who self-medicate or mix with lithium. its like playing russian roulette with your nervous system. and then they wonder why they’re exhausted all the time. its not laziness. its your muscles dissolving. and yes, i’ve read the whole thing. twice.Naresh LFebruary 8, 2026 AT 03:46
It’s fascinating how we’ve pathologized the body’s response to chemical imbalance as a psychiatric failure. But NMS isn’t a breakdown of the mind-it’s the mind witnessing the body’s rebellion against forced neurochemical suppression. We treat dopamine as if it’s a switch to flip, not a river that runs through every system. When we dam it, the flood comes. And we’re surprised when the levee breaks.Bob CohenFebruary 8, 2026 AT 07:46
lol at the people who think this is rare. i work in psych and we’ve had 4 cases in the last year alone. everyone acts like it’s a horror story but honestly? it’s just bad prescribing. if you’re jumping someone from 5mg to 15mg haloperidol in a day? you’re not a doctor. you’re a liability with a stethoscope.Ishmael brownFebruary 10, 2026 AT 05:24
so… if you stop antipsychotics too fast you can get NMS? 🤯 so like… the cure is also the poison? 🤔 maybe we should just stop giving people meds entirely? 🙃Bryan ColemanFebruary 10, 2026 AT 08:03
I’ve been on olanzapine for 5 years. No issues. But reading this? I’m gonna print this out and give it to my PCP. Just in case. Also, side note-my CK was 800 last year. Doc said it was "probably just gym." Maybe not. 🤷♂️