Anticoagulation: What It Is, Why It Matters, and How Medications Affect It
When your blood doesn’t clot the way it should, or clots when it shouldn’t, anticoagulation, the medical process of preventing dangerous blood clots using specific drugs. Also known as blood thinning, it’s not about making your blood watery—it’s about carefully balancing the system that keeps you alive. People on anticoagulants are often managing conditions like atrial fibrillation, deep vein thrombosis, or after heart valve surgery. But what most don’t realize is that everyday medications can quietly sabotage this balance.
Blood thinners, drugs like warfarin, apixaban, or rivaroxaban that reduce clotting risk don’t work in a vacuum. They’re affected by what you eat, what else you take, and even how your body breaks them down. For example, St. John’s Wort, a popular herbal supplement that speeds up liver metabolism can drop anticoagulant levels so low that clots form. On the flip side, acid-reducing medications, like PPIs used for heartburn can mess with how your body absorbs certain blood thinners, making them less effective—or more dangerous. Even grapefruit, which many think is just healthy, can interfere with how your liver processes these drugs, raising the risk of bleeding.
Anticoagulation isn’t just about popping a pill. It’s about understanding the ripple effect. A drug for cholesterol might interact with your blood thinner. A supplement for mood might cancel out your treatment. A simple change in diet could tip the scale toward a stroke or a dangerous bleed. That’s why monitoring isn’t optional—it’s life-saving. People on these meds need regular check-ins, lab tests, and honest conversations with their providers about everything they’re taking, from antibiotics to herbal teas.
What you’ll find below isn’t just a list of articles. It’s a practical guide to the hidden connections between anticoagulation and everyday meds. You’ll see how St. John’s Wort can sabotage blood thinners, why acid reducers mess with drug absorption, how liver health impacts clotting drugs, and what happens when antibiotics and anticoagulants collide. These aren’t theoretical risks—they’re real, documented, and happening right now to people who didn’t know to ask.
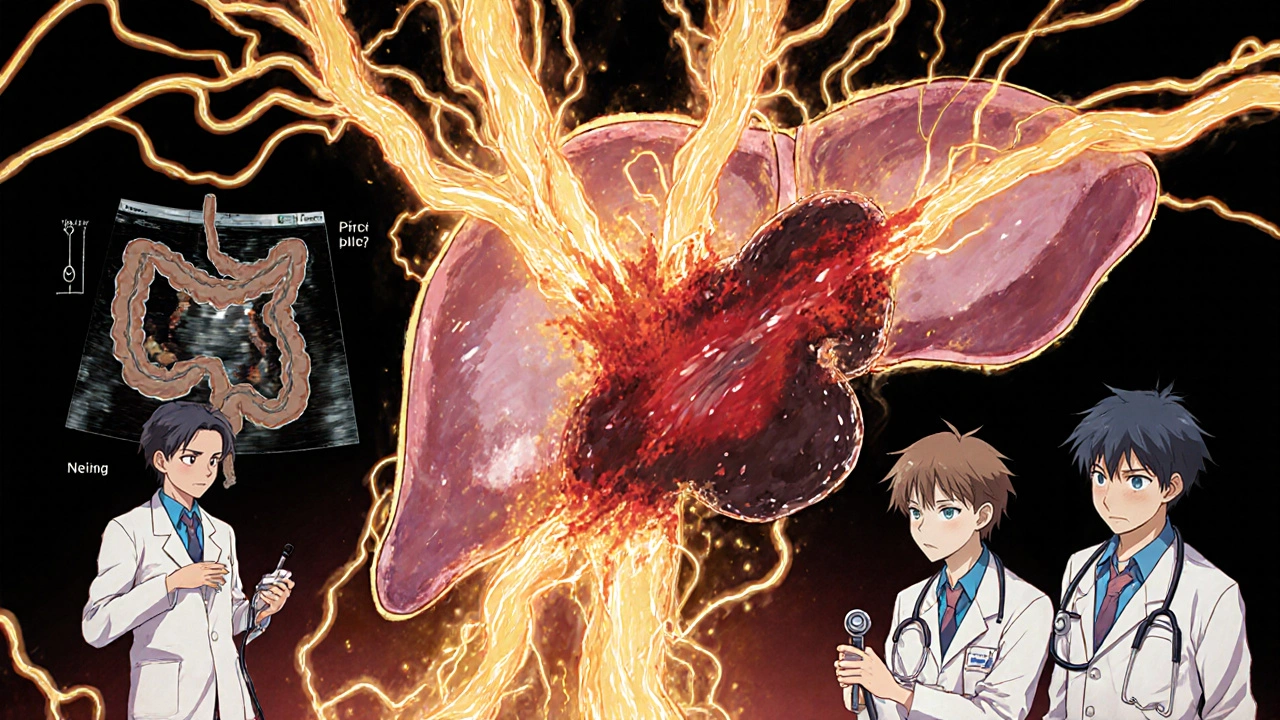
Portal vein thrombosis is a serious but treatable condition. Early diagnosis with ultrasound and timely anticoagulation can prevent complications and improve survival. Learn how to diagnose and manage PVT effectively.