ADHD – What You Need to Know and How to Manage It
When working with ADHD, Attention‑Deficit/Hyperactivity Disorder, a neurodevelopmental condition that shows up as chronic inattention, impulsivity, and hyperactivity. Also known as Attention Deficit Disorder, it affects kids, teens, and many adults throughout their lives. Understanding ADHD helps you spot the right support, whether it’s medication, therapy, or lifestyle tweaks.
One of the biggest decisions is choosing a stimulant medication, drugs like methylphenidate or amphetamine that increase dopamine and norepinephrine activity in the brain. These meds are often the first line because they work fast and improve focus for a large share of people. However, they aren’t a one‑size‑fits‑all, and some folks prefer a non‑stimulant option, such as atomoxetine, which targets the same neurotransmitters without the classic stimulant profile. Both categories have benefits and side‑effects, so a thorough medical review and trial period are key.
Medication isn’t the whole story. Cognitive Behavioral Therapy, a structured, skills‑focused therapy that teaches coping strategies and thought restructuring works hand‑in‑hand with meds to tackle impulsivity and poor planning. CBT helps you build routines, break down tasks, and manage the emotional fallout of missed deadlines or criticism. When combined with behavioral coaching, the gains can be lasting even after the medication dose is reduced.
Beyond meds and therapy, improving executive function, the set of mental skills for organizing, prioritizing, and regulating behavior is a daily priority. Simple tools like timer apps, visual planners, and ‘one‑thing‑at‑a‑time’ checklists can rewire habits over weeks. Research shows that consistent practice of these strategies reduces procrastination and boosts academic or work performance, no matter the age.
Putting It All Together
Diagnosing ADHD involves a structured interview, rating scales, and sometimes neuropsychological testing to rule out other conditions. A clear diagnosis sets the stage for a personalized treatment plan that blends medication, therapy, and executive‑function coaching. You’ll also want to involve teachers, employers, or family members so everyone understands the plan and can provide consistent support.
Below you’ll find a curated list of articles that walk through each of these pieces in detail – from selecting the right stimulant to mastering CBT techniques, from managing side‑effects to building daily habits that stick. Dive in and pick the insights that match where you are on your ADHD journey.
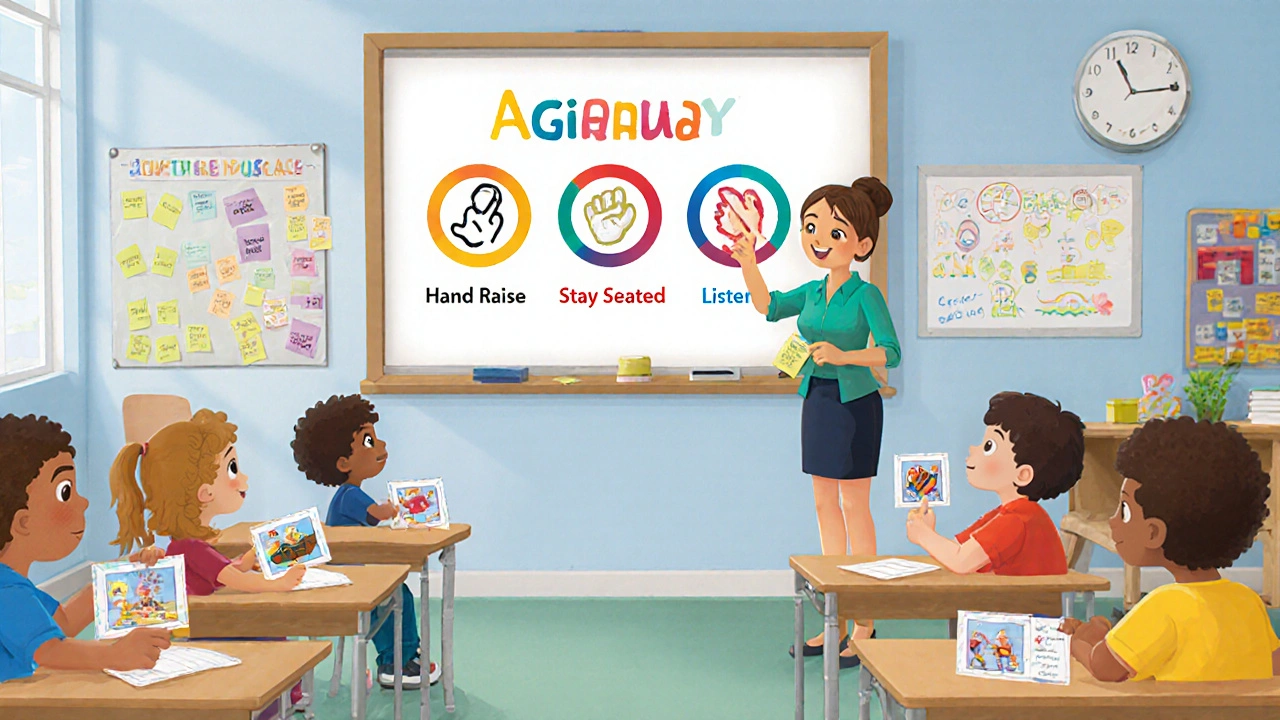
Learn practical, tiered strategies to handle classroom behavior disorders, from early spotting to individualized plans, with real examples and data tools.