Skin Condition & Tattoo Risk Calculator
Your Risk Assessment
Recommendations
Skin Condition Information
Eczema
Chronic inflammatory condition causing dry, itchy skin. Can lead to uneven ink retention and increased infection risk.
Psoriasis
Autoimmune disorder causing thick, scaly patches. May result in patchy coloration and longer healing times.
Acne
Clogged pores causing pimples. Active breakouts can become infected post-tattoo and distort design.
Keloid-prone
Excessive scar tissue formation after injury. Tattooing can cause raised, firm keloids around the design.
Ink Allergy
Immune response to pigments. Symptoms may appear weeks later as rashes, swelling, or blistering.
Key Takeaways
- Identify any existing skin condition before booking a session.
- Talk to a qualified tattoo artist and a dermatologist about your skin health.
- Follow a tailored pre‑ink and aftercare routine to minimize irritation.
- Know which pigments are more likely to trigger allergic reactions.
- Watch for signs of infection or flare‑ups during the healing period.
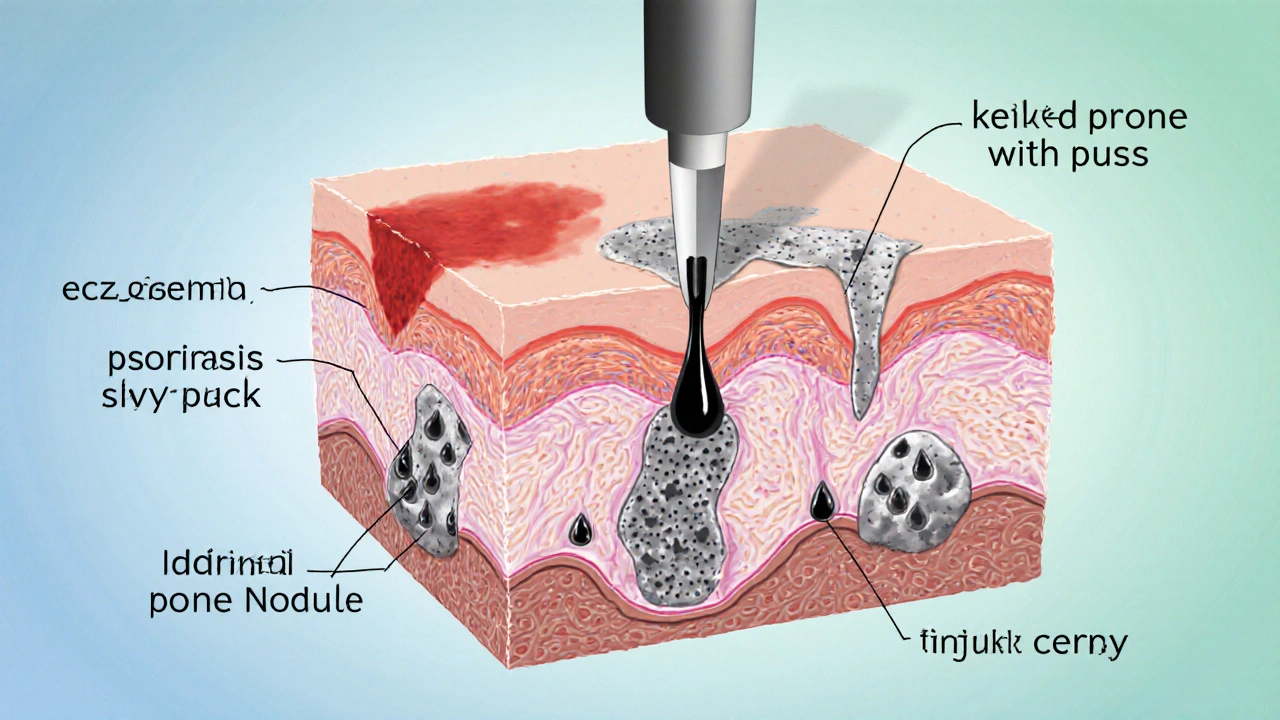
Understanding Tattoo is a permanent design placed under the skin using ink and needles
People choose tattoos for personal expression, cultural reasons, or simply because they look cool. The process involves puncturing the dermis - the second layer of skin - so the ink stays visible for life. While the art itself is straightforward, the skin’s condition before, during, and after the session plays a huge role in how well the design heals.
Common Skin Conditions That Affect Tattooing
Below are the most frequent conditions that can clash with inkwork. Each entry includes a brief definition and the specific concerns it raises for a tattoo session.
Eczema is a chronic inflammatory skin disorder that causes itching, redness, and scaling. When the skin is actively flaring, the barrier is compromised, making it harder for ink to settle and more likely to trigger a severe reaction.
Psoriasis is an autoimmune condition that speeds up skin cell turnover, leading to thick, scaly plaques. Tattoos placed over plaques may experience uneven ink absorption and a higher chance of scar formation.
Acne is a condition where hair follicles become clogged with oil and dead skin cells, creating pimples and cysts. Active breakouts can become infected after a needle puncture, and scar tissue may distort the final design.
Keloid‑prone skin is a tendency for the skin to produce excess fibrous tissue after injury, resulting in raised, firm scars. Since tattooing is a controlled injury, people who scar keloidally often end up with raised bumps around the ink.
Ink allergy is an immune response to pigments, most commonly red, yellow, or certain black inks. Symptoms range from mild itching to blistering and can appear weeks after the tattoo.
How Skin Conditions Change the Tattoo Process
- Consultation step - the artist should ask about any diagnosed condition, medication, or recent flare‑ups.
- Patch test - a small dot of the chosen pigment placed on an inconspicuous area to watch for an allergic response over 48‑72 hours.
- Needle depth adjustment - for sensitive or inflamed skin, a shallower needle setting reduces trauma.
- Session length - breaking a large piece into shorter appointments helps the skin recover between sessions.
- Aftercare modifications - using fragrance‑free, barrier‑supporting ointments instead of standard petroleum jelly.
Preparing Your Skin Before Getting Inked
- Schedule a dermatologist visit at least two weeks before your tattoo date. Ask for a clearance note that outlines any needed medication pauses (e.g., topical steroids). \n
- Hydrate your skin daily with a plain, hypoallergenic moisturizer. Avoid retinoids, benzoyl peroxide, or strong exfoliants for at least a week.
- If you have eczema, keep flare‑ups under control with prescribed creams. A flare‑free week is ideal before the needle touches your skin.
- Stay away from alcohol and non‑steroidal anti‑inflammatory drugs (NSAIDs) 48 hours before the session to reduce bleeding risk.
- Discuss pigment choices with the artist. Opt for organic or vegetable‑based inks if you’ve shown sensitivity to metal‑based pigments.
Aftercare Tailored to Sensitive Skin
Standard tattoo aftercare-soap, water, and a thin layer of ointment-works for most people, but those with skin conditions need an extra layer of protection.
- Cleanse with a mild, fragrance‑free antibacterial wash (e.g., chlorhexidine 0.05%). Do this twice a day for the first week.
- Apply a silicone‑based gel sheet after the first 48 hours if you’re prone to keloids. Silicone helps flatten raised tissue.
- For eczema or psoriasis, use a barrier cream containing ceramides after the wound has closed (usually day 5‑7). This restores the skin’s lipid layer.
- Monitor for signs of infection - increasing redness, warmth, pus, or a fever. Contact a medical professional promptly.
- Avoid sun exposure and tight clothing over the fresh tattoo for at least four weeks. UV rays can exacerbate pigment allergies and trigger flare‑ups.
When to Consult a Dermatologist
Even with careful preparation, complications can arise. Here are red flags that warrant a professional eye.
- Persistent swelling or pain beyond the first three days.
- Development of a raised, firm scar that continues to enlarge (possible keloid).
- Itching or rash that spreads beyond the tattoo borders, suggesting a systemic allergic reaction.
- New or worsening lesions of psoriasis or eczema that appear at the tattoo site.
- Any sign of infection - especially if you have a compromised immune system.
The dermatologist can prescribe topical steroids, antihistamines, or, in rare cases, recommend laser removal of the problematic pigment.
Comparison: Skin Condition vs Tattoo Risk
| Condition | Impact on Ink Retention | Healing Time | Special Aftercare |
|---|---|---|---|
| Eczema | Potential uneven pigment if skin is dry or inflamed | 10‑14 days (may extend if flare‑up occurs) | Moisturizer with ceramides; avoid scratching |
| Psoriasis | Scaly plaques can cause patchy coloration | 12‑21 days (longer with plaques) | Gentle steroid ointment after wound closure |
| Acne‑prone skin | Active pimples may lead to infection and distortion | 7‑10 days (if no cystic acne develops) | Antibacterial wash; avoid touching the area |
| Keloid‑prone | Ink may be surrounded by raised fibrous tissue | 15‑30 days (scar maturation can take months) | Silicone gel sheets; pressure therapy if needed |
| Ink allergy | Localized rash, swelling, or blistering | Variable - may require medical intervention | Patch test beforehand; antihistamines if reaction occurs |
Frequently Asked Questions
Can I get a tattoo if I have eczema?
Yes, but only when the condition is well‑controlled. A dermatologist should confirm that the skin isn’t actively flaring, and the artist should use a shallow needle depth and a fragrance‑free aftercare routine.
What pigment should I avoid if I have a history of allergies?
Red and yellow pigments often contain mercury sulfide or cadmium and are the most common culprits. Opt for black or grey inks made from iron oxide, or ask the artist for a hypoallergenic, vegan‑based pigment.
How long should I wait after a psoriasis flare before getting inked?
Wait at least two weeks after the flare subsides and the skin looks normal. This gives the epidermal barrier time to rebuild, reducing the risk of uneven color.
Is it safe to tattoo over a keloid scar?
Generally not recommended. The scar tissue is already over‑producing collagen; adding more trauma can make the keloid larger. If you must, discuss laser‑softening of the scar with a dermatologist first.
What signs indicate I need medical attention after a tattoo?
Look for spreading redness, increasing pain, pus, fever, or a rash that doesn’t improve after a few days. Any of these symptoms should prompt a visit to a healthcare professional.


11 Comments
Jillian BellOctober 9, 2025 AT 23:24
Ever notice how the tattoo industry keeps pushing pigments that are basically industrial waste? They’re disguised as “organic” but the supply chain is riddled with secret additives that could trigger an autoimmune flare. If you’re already dealing with eczema or psoriasis, you’re basically signing a contract with your own immune system. Keep your skin guard up and demand full disclosure before you sit in the chair.
Lindsey BolligOctober 10, 2025 AT 00:31
Great rundown! If you’ve got a mild flare, try calming your skin with a fragrance‑free moisturizer a week before the session. Schedule a quick check‑up with your dermatologist to get the green light – it’s worth the extra appointment. When you’re in the studio, let the artist know about any sensitivities so they can adjust needle depth. After the tattoo, stick to a gentle, fragrance‑free aftercare ointment and you’ll be golden.
Daniel BuchananOctober 10, 2025 AT 01:38
Everyone, remember that tattooing is a collaborative process between you, the artist, and sometimes a medical professional. If you have a condition like keloid‑prone skin, a brief consultation with a dermatologist can help you decide on pre‑emptive silicone sheets. Choose an artist who respects your medical history and is willing to adapt their technique. This partnership can keep the healing process smooth and reduce the chance of unexpected scarring.
Lena WilliamsOctober 10, 2025 AT 02:44
i was thinkin bout gettin a new piece and readin that guide got me real curious lol. the thing is, when u got acne its not just about poppin pimples, the bacteria can mess with the ink cloudin it up afterwards. also, if your skin is dry from eczema u might see the colors look kinda faded cuz the barrier is all cracked. i heard some artists use a shallower depth for sensitive skins but not all of them get that right, some just ignore the warning signs. u gotta be real careful and maybe do a tiny patch test on an area you wont notice, like behind the ear, just to see if any rash pops up. honestly, taking the extra step can save u from a lotta regret later on, trust.
Sierra BagstadOctober 10, 2025 AT 03:51
When considering a tattoo with an underlying dermatologic condition, it is essential to approach the decision methodically. First, obtain a comprehensive assessment from a board‑certified dermatologist to document the status of the skin condition. Second, ensure that any active flare‑ups have been medically managed and are in remission for a minimum of two weeks. Third, discuss the planned tattoo with the artist, emphasizing the need for a shallow needle depth and minimal dwell time. Fourth, request that the artist perform a pigment patch test on an inconspicuous area and observe the site for at least 72 hours. Fifth, choose inks that are free from known allergenic metals such as mercury, cadmium, and nickel, opting instead for iron‑oxide–based pigments when possible. Sixth, avoid topical retinoids, benzoyl peroxide, and other irritants for at least one week prior to the appointment. Seventh, maintain optimal skin hydration with a fragrance‑free, ceramide‑rich moisturizer in the days leading up to the session. Eighth, abstain from alcohol and non‑steroidal anti‑inflammatory drugs 48 hours before tattooing to reduce bleeding risk. Ninth, after the procedure, cleanse the area twice daily with a mild, antiseptic cleanser such as chlorhexidine 0.05 %. Tenth, apply a thin layer of a silicone‑based gel sheet after the initial 48‑hour period if the client is prone to keloid formation. Eleventh, for eczema or psoriasis, transition to a barrier cream containing ceramides once the wound has epithelialized, typically around day five to seven. Twelfth, monitor the tattoo for signs of infection, including increasing erythema, warmth, purulent discharge, or systemic symptoms such as fever. Thirteenth, if any allergic reaction emerges, administer a second‑generation antihistamine and seek medical evaluation promptly. Fourteenth, avoid direct sun exposure and tight clothing over the tattoo for at least four weeks to prevent pigment degradation and flare‑ups. Finally, schedule a follow‑up dermatology visit within six weeks to assess healing progress and intervene if atypical scarring or pigment changes occur. By adhering to this systematic protocol, individuals with pre‑existing skin conditions can significantly mitigate risks and achieve satisfactory tattoo outcomes.
Alan KogosowskiOctober 10, 2025 AT 04:58
There’s a common misconception that any healthy‑looking skin can tolerate a tattoo without issue. In reality, subclinical inflammation can still affect ink retention and healing time. For instance, someone with a history of mild psoriasis may have patches that appear clear but are still undergoing accelerated keratinocyte turnover. This can result in uneven coloration that only becomes apparent after the initial healing phase. Moreover, pigment composition matters; certain azo dyes have been linked to delayed hypersensitivity reactions. A pragmatic approach is to combine a dermatologist’s clearance with the artist’s technical adjustments, such as using a smaller needle grouping. Ultimately, the goal is to balance artistic ambition with biomedical prudence.
Ben LeeOctober 10, 2025 AT 06:04
I totally get that getting ink can feel like a big leap, especially when you’ve got skin that’s a bit tricky. It’s cool to see you doing the homework and looking into aftercare tweaks. If you’re dealing with keloids, the silicone gel sheets really help flatten the tissue over time. For eczema, a ceramide‑rich moisturizer after the wound closes will keep the barrier strong. Talk to your artist about using a shallower needle depth; it reduces trauma and speeds up recovery. Pair that with a fragrance‑free ointment for the first few days and you’ll likely avoid a lot of irritation. Keep an eye on the tattoo as it heals and adjust your routine if anything feels off.
David BriceOctober 10, 2025 AT 07:11
Listen up, if you’re ignoring the medical advice and just jumping in because “it looks cool,” you’re begging for a disaster. Get that skin checked, even if you think you’re fine-keloid‑prone folks end up with a raised scar that looks like a mountain. Use the patch test, stop using the heavy‑duty antibiotic ointments that can actually dry out your skin, and switch to a silicone gel asap. Don’t be a hero by skipping the dermatologist; the point is to keep the ink from becoming a permanent problem. Your aftercare must be consistent, not just a “spray‑and‑go” mess. If you see any redness after day three, act fast-don’t wait till it’s a full‑blown infection. This isn’t a suggestion, it’s a survival plan.
Zachary SchroerOctober 10, 2025 AT 08:18
Honestly tattoos are just modern body branding 🤷♂️ the hype about skin conditions is overblown – your immune system is robust enough 💅
Mina BerensOctober 10, 2025 AT 09:24
Great info, definitely will share! 👍
Moritz BenderOctober 10, 2025 AT 10:31
From a pharmacokinetic perspective, dermal absorption of metal‑based pigments can elicit a type IV hypersensitivity response, especially in patients with prior atopic dermatitis. Utilizing hypoallergenic organics mitigates the hapten‑carrier complex formation, thereby reducing the odds of a delayed eczematous reaction. Post‑procedure, a non‑comedogenic barrier repair ointment with niacinamide can reinforce the stratum corneum while modulating inflammatory cytokine release. 📈