Drug Interaction Checker: Spot Dangerous Combinations
This tool helps identify potentially dangerous drug combinations based on the most lethal interactions documented in healthcare. Enter medications you're taking to see if they form a known dangerous combination. Always consult your pharmacist or doctor for medical advice.
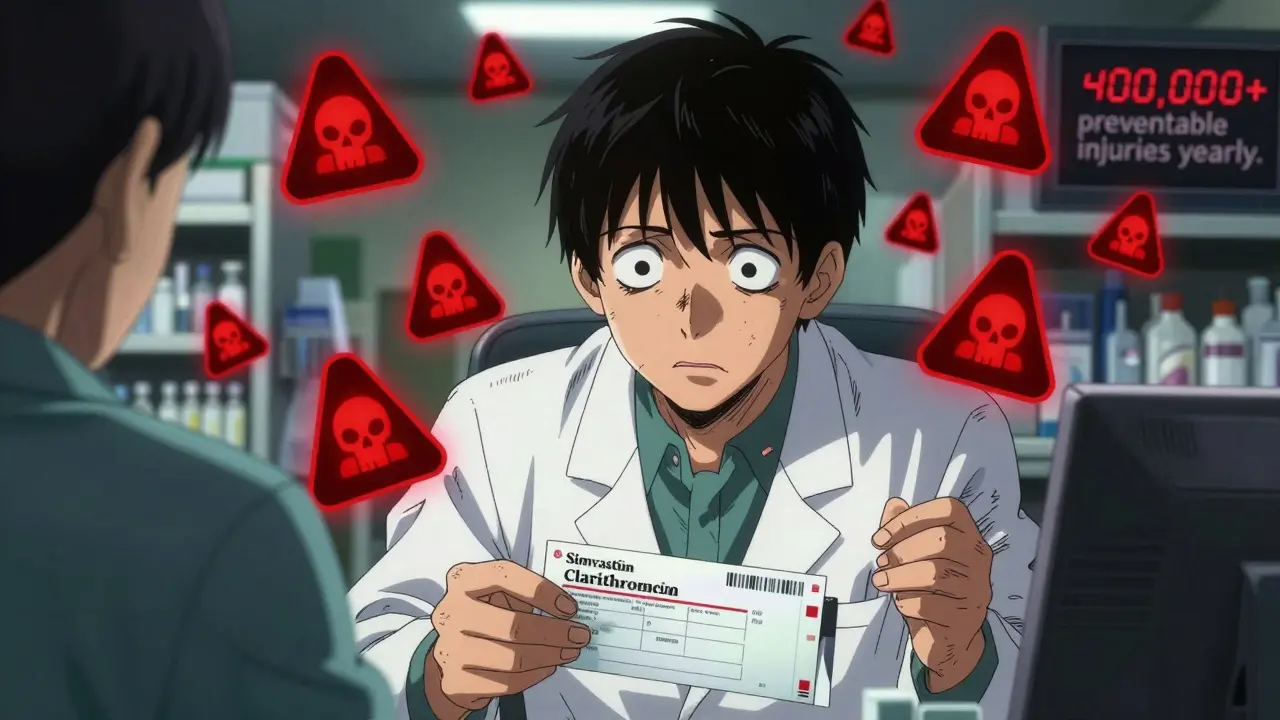
Every year, over 400,000 preventable drug-related injuries happen in U.S. hospitals alone. Many of these aren’t random mistakes-they’re avoidable clashes between medications that should have been caught before they reached the patient. And the person who’s supposed to catch them? The pharmacist. But too often, they’re drowning in alerts, missing the ones that actually matter.
What Makes a Drug Interaction a Red Flag?
Not all drug interactions are created equal. Some cause mild nausea. Others can kill you in hours. A red flag interaction is one where the risk isn’t just theoretical-it’s proven, deadly, and well-documented. These aren’t "maybe" situations. They’re "don’t do this" situations.The Chicago Tribune’s 2016 investigation tested 255 pharmacies across Chicago with five known dangerous combinations. In more than half of those cases, pharmacists didn’t warn patients. That’s not a glitch. That’s a system failure.
Here’s what actually kills:
- Tizanidine + Ciprofloxacin: One relaxes muscles. The other fights infection. Together, they shut down your brain’s ability to stay awake. Patients have passed out, fallen, and suffered head trauma.
- Colchicine + Verapamil: Used for gout and high blood pressure. Combined, they cause toxic buildup in your muscles and organs. Death from multi-organ failure has been reported.
- Simvastatin + Clarithromycin: One lowers cholesterol. The other treats pneumonia. Together, they shred muscle tissue. Creatine kinase levels can spike over 10,000 U/L-normal is under 200. Kidney failure follows fast.
- Clarithromycin + Ergotamine: This combo causes ergotism-a condition where blood vessels constrict so severely that fingers and toes turn black and die. Some patients lose limbs.
- Birth control + Griseofulvin: An antifungal that makes birth control useless. Pregnancy rates jump past 30%. And if you get pregnant? Risk of serious birth defects skyrockets.
These aren’t edge cases. They’re repeat offenders. And they keep happening because the system isn’t built to stop them.
Why Pharmacists Miss These Dangers
It’s not that pharmacists don’t care. It’s that they’re flooded.Computer systems throw up alerts for every possible interaction-even ones that barely matter. A patient on aspirin and ibuprofen? Alert. A patient on a common antibiotic and a vitamin? Alert. A patient on two drugs that could cause sudden death? Sometimes, that gets lost in the noise.
This is called "alert fatigue." Pharmacists see hundreds of warnings a day. After a while, they start clicking "ignore" without reading. It’s human. It’s predictable. And it’s deadly.
Professor John Horn from the University of Washington School of Pharmacy studied this for years. He worked with 12 major health systems to redesign their alert systems. Result? They cut irrelevant alerts by 78%. And suddenly, pharmacists started catching the dangerous ones-up to 89% of them, instead of 48%.
The fix isn’t more alerts. It’s smarter alerts.
The Real-World Cost of Missing a Warning
A 68-year-old man with atrial fibrillation was prescribed warfarin to prevent strokes. Then he got pneumonia and was given amiodarone. His doctor didn’t know the interaction. His pharmacist didn’t catch it.Amiodarone blocks the enzymes that break down warfarin. Blood levels of warfarin soared. He started bleeding internally. He ended up in the ICU. He survived-but barely. His INR, a measure of blood thinning, hit 12. Normal is 2 to 3.
That’s not rare. The American Academy of Family Physicians says this exact combo requires a 30-50% warfarin dose reduction and weekly INR checks for weeks. But most pharmacies don’t have protocols to enforce it.
Same with digoxin and verapamil. Together, they slow the heart so much it can stop. Serum digoxin levels can rise by 60-75%. EKG changes show up fast. But without a pharmacist checking, it’s just another prescription filled.
And it’s not just the elderly. Children, pregnant women, and people with liver or kidney disease are at higher risk. The FDA says 35% of all adverse drug events happen in people over 65. They’re taking an average of 4.5 prescriptions a day. Each one is a potential landmine.
What Pharmacists Should Be Doing-But Often Aren’t
There’s a clear checklist for what needs to happen when a high-risk combo is flagged:- Identify the combo: Know the top 10 lethal interactions cold. Simvastatin + clarithromycin? Red flag. Warfarin + amiodarone? Red flag. Birth control + griseofulvin? Red flag.
- Assess the patient: Is this person over 65? Do they have kidney disease? Are they pregnant? Risk isn’t the same for everyone.
- Check for alternatives: Can you switch simvastatin to pravastatin? Can you swap clarithromycin for azithromycin? Sometimes, there’s a safer option.
- Call the prescriber: Don’t just warn the patient. Call the doctor. Say: "This combo could cause rhabdomyolysis. Can we change the antibiotic?"
- Document and follow up: If you dispense it anyway, make sure the patient knows the signs of trouble-muscle pain, dark urine, dizziness, irregular heartbeat. Tell them to come back immediately if they feel off.
But here’s the problem: most community pharmacies process a prescription in 2.3 minutes. That’s not enough time to do all of this. And most don’t have AI tools or tiered alert systems to help.
What You Can Do to Protect Yourself
You can’t rely on the system. You have to be your own advocate.- Know your meds: Keep a list of every pill, patch, and injection you take-including over-the-counter drugs and supplements. Bring it to every appointment.
- Ask the pharmacist: When you pick up a new prescription, say: "Is this safe with everything else I’m taking?" Don’t wait for them to ask you.
- Know your red flags: If you’re on simvastatin and get an antibiotic, ask if it’s clarithromycin or erythromycin. If yes, say no. Ask for azithromycin instead.
- Use one pharmacy: If you get all your meds from one place, they can build a full picture of your regimen. Splitting prescriptions between pharmacies is a recipe for missed interactions.
- Speak up if something feels wrong: Muscle pain, dark urine, dizziness, irregular heartbeat, unexplained bruising-these aren’t normal side effects. They’re warning signs. Get checked.
The Future: Can Technology Fix This?
The FDA’s 2023-2025 Digital Health Plan is funding AI tools that don’t just check drug pairs. They look at your age, kidney function, liver enzymes, genetics, and even your diet. One tool can predict if a patient on warfarin will bleed after adding a new statin-not just guess, but calculate risk based on real data.Some hospitals are already using these. But most community pharmacies? Still stuck with the same 2010-era software.
The CDC says mandatory pharmacist counseling for high-risk prescriptions could prevent 150,000 adverse events a year. But that requires time, training, and funding. Right now, pharmacies are pressured to fill scripts fast, not to save lives slow.
Without systemic change-better alerts, more staffing, smarter tech-this problem will get worse. The National Academy of Medicine predicts a 27% increase in adverse drug events by 2030. More people. More meds. Same broken system.
Bottom Line: Don’t Assume It’s Safe
Pharmacists are trained to catch these things. But the system is designed to let them fail. That’s not their fault. It’s the system’s.If you’re taking more than three medications, you’re at risk. If you’re over 65, you’re at higher risk. If you’re on statins, blood thinners, or birth control, you’re in the danger zone.
Don’t wait for someone else to protect you. Know your meds. Ask the questions. Push for alternatives. If your pharmacist doesn’t know about the interaction between your gout pill and your heart medicine, find someone who does.
Your life isn’t a data point. It’s not an alert. It’s yours. And you deserve to take your meds without fear.
What are the most dangerous drug combinations I should watch out for?
The most lethal combinations include simvastatin with clarithromycin (risk of muscle breakdown and kidney failure), colchicine with verapamil (toxic buildup), tizanidine with ciprofloxacin (loss of consciousness), clarithromycin with ergotamine (tissue death), and birth control with griseofulvin (pregnancy and birth defects). Warfarin with amiodarone can cause dangerous bleeding, and digoxin with verapamil can cause heart block. These are not rare-they’re documented, preventable, and deadly.
Why do pharmacists sometimes miss these dangerous interactions?
Pharmacists face "alert fatigue"-they’re bombarded with hundreds of warnings daily, most of which are low-risk. Systems aren’t smart enough to prioritize life-threatening combos. As a result, critical alerts get ignored. Studies show over half of dangerous interactions go uncaught in community pharmacies because the software doesn’t filter by severity.
Can I trust my pharmacist to catch all dangerous interactions?
You can’t assume they will. Even with training and software, the system is overloaded. A 2016 investigation found 52% of pharmacies failed to warn patients about known deadly interactions. Your pharmacist is a professional, but they’re working under impossible conditions. Always ask: "Is this safe with everything else I take?"
What should I do if I’m prescribed a drug that might interact with my current meds?
Don’t fill the prescription until you’ve spoken to both your doctor and pharmacist. Ask if there’s a safer alternative-like switching from clarithromycin to azithromycin, or from simvastatin to pravastatin. If they say it’s fine, ask for evidence. If you’re on blood thinners, statins, or birth control, assume every new drug needs scrutiny.
Are over-the-counter drugs and supplements safe to mix with prescriptions?
No. St. John’s wort can make birth control fail. Grapefruit juice can turn statins toxic. NSAIDs like ibuprofen can increase bleeding risk with warfarin. Even "natural" supplements can cause serious interactions. Always list everything you take-including vitamins, herbs, and CBD-when talking to your pharmacist.
How can I reduce my risk of dangerous drug interactions?
Use one pharmacy for all your prescriptions. Keep an updated list of every medication and supplement you take. Bring it to every appointment. Ask your pharmacist to review it every time you get a new script. If you’re over 65 or taking more than four meds, schedule a medication review with your pharmacist at least once a year.

12 Comments
Doug GrayJanuary 29, 2026 AT 07:44
Look, I get it-pharmacists are overworked. But let’s be real: if your system throws 300 alerts a day and half are "ibuprofen + aspirin?" then the problem isn’t human error, it’s software designed by people who’ve never met a patient. Alert fatigue? More like alert absurdity. We’re automating bureaucracy, not safety.
Kristie HorstJanuary 30, 2026 AT 01:38
How tragic that we’ve turned the guardians of pharmaceutical safety into clickers of "ignore" buttons. One wonders if the FDA’s digital health plan will include a mandatory 10-minute pause before any alert can be dismissed. Or perhaps we could just… hire more pharmacists? Just a thought.
Laia FreemanJanuary 30, 2026 AT 12:58
OMG YES!!! I got prescribed clarithromycin last year and my pharmacist was like "ohhh yeah that’s bad with your simva" and I was like THANK YOU GOD. I’ve been using one pharmacy since 2020 and I swear it saved my life!!! 🙏💊Keith OliverJanuary 30, 2026 AT 15:24
You’re all missing the point. This isn’t about pharmacists or alerts. It’s about the pharmaceutical-industrial complex weaponizing complexity to maintain profit margins. If every interaction were flagged and managed properly, generics would be obsolete. This is engineered obsolescence disguised as healthcare.
Kacey YatesJanuary 31, 2026 AT 15:22
Griseofulvin kills birth control? I knew someone who got pregnant on that and blamed the pill. No. It was the fungus treatment. Don't be that person. Always tell your pharmacist EVERYTHING. Even that ginseng tea you think is harmless.ryan SifontesFebruary 1, 2026 AT 10:36
they're watching you. every pill you take. every alert you ignore. the system knows. they're not fixing it because they need the ER visits. the data. the profits. you think this is an accident? no. it's a feature.Laura ArnalFebruary 1, 2026 AT 14:41
I’m so glad this got posted! My grandma almost lost a foot because of ergotamine + clarithromycin. She’s fine now but we had to fight for weeks to get her meds right. You’re not paranoid if the system is broken. 💪❤️Jasneet MinhasFebruary 1, 2026 AT 17:15
It is quite remarkable how the American healthcare model prioritizes throughput over patient safety. In India, pharmacists are legally required to counsel patients on all new prescriptions. The outcome? Far fewer adverse events. Perhaps we should consider a paradigm shift rather than merely tweaking broken software.
Eli InFebruary 1, 2026 AT 18:56
I’m from a rural town and our pharmacist is the only one who knows everyone’s meds. She remembers my dad’s warfarin, my mom’s diabetes meds, and even my CBD oil. We don’t need AI-we need people who care. 🌿❤️Megan BrooksFebruary 3, 2026 AT 04:12
The structural constraints placed upon community pharmacy practice are profound. One cannot reasonably expect a clinician to perform a comprehensive medication review in 2.3 minutes while simultaneously managing insurance denials, refill requests, and regulatory compliance. The issue is systemic, not individual.
Ryan PaganFebruary 3, 2026 AT 04:52
Let’s stop pretending this is just about software. This is about greed wrapped in a white coat. Pharmacies are corporations. They pay pharmacists peanuts to move scripts fast. That’s why you get the "click ignore" reflex. They don’t care if you live or die-they care if you come back next week for your statin refill. It’s capitalism with a stethoscope.
Paul AdlerFebruary 4, 2026 AT 13:15
This is a deeply important conversation. I’ve seen firsthand how alert fatigue erodes clinical judgment-not because pharmacists are careless, but because they’ve been conditioned to respond to noise as if it were signal. The solution isn’t more alerts. It’s better signal detection. And that requires investment-not just in tech, but in time, training, and trust.