When you're pregnant or breastfeeding and need psychiatric medication, you're not just managing your mental health-you're managing two lives. That’s why coordinating care between your OB/GYN and psychiatrist isn’t just helpful-it’s essential. Too often, women get caught in the middle: their OB/GYN says one thing about medication safety, their psychiatrist says another, and no one talks to each other. The result? Unnecessary stress, medication changes that don’t make sense, or worse-stopping treatment altogether when it’s needed most.
Why Coordination Isn’t Optional
About 1 in 5 women experience depression, anxiety, or bipolar disorder during pregnancy or after giving birth. Left untreated, these conditions raise the risk of preterm birth, low birth weight, and even postpartum suicide. But the same medications that help you feel like yourself again can raise questions about safety for your baby. That’s where coordination kicks in. The American College of Obstetricians and Gynecologists (ACOG) made it clear in 2023: treating mental illness during pregnancy isn’t a choice between two risks-it’s about balancing both. The biggest danger? Not taking medication when it’s needed. Untreated severe depression increases the chance of preterm birth by 40% and low birth weight by 30%. The goal isn’t to avoid all medication-it’s to use the right one, at the right dose, at the right time.Which Medications Are Safest?
Not all antidepressants are created equal when you’re pregnant or breastfeeding. Research shows some have far better safety records than others.- Sertraline is the top choice. It crosses the placenta minimally, has very low levels in breast milk, and shows no significant increase in birth defects. Studies tracking over 15,000 pregnancies found only a 0.5% absolute risk increase for heart defects-barely higher than the 1% baseline risk in the general population.
- Escitalopram is a close second. It’s also well-studied, with minimal transfer to the baby and low risk of neonatal withdrawal symptoms.
- Paroxetine is not recommended. Even though it works for some, it’s linked to a slightly higher risk of heart defects and should be avoided if possible.
- Mood stabilizers like lithium can be used in bipolar disorder, but require close monitoring. Valproate, however, is a hard no-it carries a 10.7% risk of major birth defects.
How the Coordination Process Actually Works
This isn’t just about sending a referral. Effective coordination follows a clear, step-by-step structure.- Preconception planning-If you’re trying to get pregnant, meet with both providers at least 3 to 6 months ahead. This is the best time to adjust meds, switch to safer options, or stabilize your dose before conception.
- First joint check-in by 8-10 weeks-That’s when your baby’s organs are forming. Both providers should review your current meds, dosages, and mental health history together.
- Regular updates every 4 weeks-Pregnancy changes how your body processes drugs. Blood volume increases by 40-50%, and your liver metabolizes meds faster, especially in the third trimester. Doses may need adjusting.
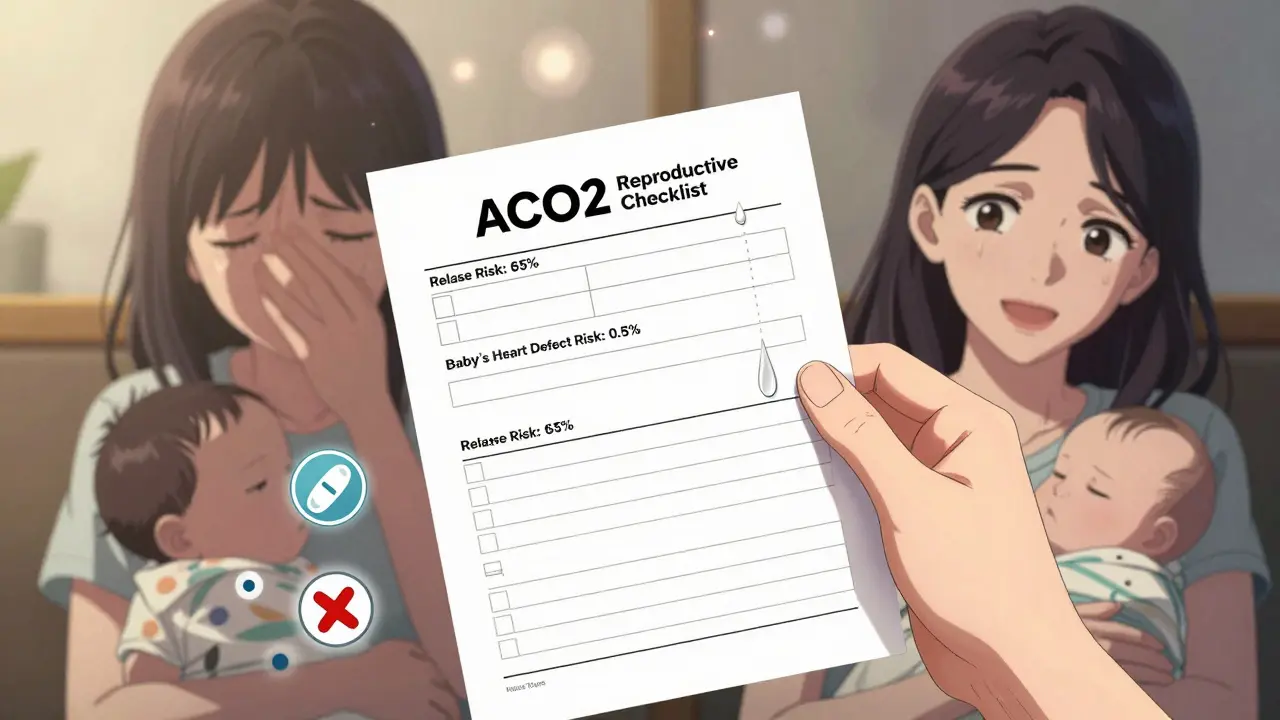
- Use a shared checklist-ACOG’s Reproductive Safety Checklist rates risks on a 1-10 scale for both relapse and medication exposure. It turns abstract fears into concrete numbers: “Without treatment, your chance of relapse is 65%. With sertraline, your baby’s risk of heart defect is 0.5%.”
- Document everything in both records-If your OB/GYN and psychiatrist use different electronic systems, ask for printed summaries. Many providers still report communication gaps because their systems don’t talk to each other.
What Happens After Baby Is Born?
Breastfeeding doesn’t mean you have to stop your meds. Most SSRIs, especially sertraline, appear in breast milk at trace levels-often lower than what the baby was exposed to in the womb. The National Pregnancy Registry for Psychiatric Medications tracks outcomes from over 15,000 pregnancies and breastfeeding cases. Their 2023 data shows no increased risk of developmental delays or behavioral issues in babies exposed to sertraline or escitalopram through breast milk. But here’s the catch: your body changes after birth. Hormones drop fast. Your medication needs may shift again. Many women feel fine during pregnancy, then crash after delivery. That’s why follow-ups at 2, 6, and 12 weeks postpartum are critical. Your psychiatrist should be involved in adjusting your dose-not your OB/GYN alone.Common Barriers and How to Get Around Them
Even with solid guidelines, real-world coordination still falls short.- Insurance delays-57% of privately insured women wait more than 14 days for prior authorization to see a psychiatrist. Call your insurer early. Ask your OB/GYN to write a letter of medical necessity. Many practices now have care coordinators who handle this for you.
- Electronic health record (EHR) gaps-67% of providers say their systems don’t share data. If your OB/GYN uses Epic and your psychiatrist uses Cerner, ask for a printed summary to hand-deliver or fax.
- Conflicting advice-On Reddit’s r/PPD community, 68% of users reported getting mixed messages. One woman stopped sertraline after her OB/GYN said it was “risky,” then developed severe postpartum depression. She ended up hospitalized. Don’t let conflicting advice stop you. Ask both providers to explain their reasoning. If they can’t agree, request a joint appointment.
When to Push for a Joint Appointment
You don’t have to wait for your providers to suggest it. If you’re on mood stabilizers, have a history of bipolar disorder, or are struggling with treatment-resistant depression, insist on a shared visit. Kaiser Permanente’s integrated model shows 89% patient satisfaction when both specialists meet together-either in person or via video. During these meetings, ask:- “What’s the risk of relapse if I stop this medication?”
- “What’s the actual risk to my baby, not just ‘it might be risky’?”
- “Can we use the Reproductive Safety Checklist to score this together?”
- “Will you both update each other’s records after this visit?”
The Future Is Getting Better
Change is happening. In January 2024, the FDA updated prescribing labels for psychiatric meds to include direct recommendations for OB/GYN coordination. Sertraline’s label now says: “Coordination with obstetric provider recommended for dose adjustment beginning at 20 weeks due to increased clearance.” Hospitals are catching up too. Epic Systems launched its Perinatal Mental Health Module in early 2023. When an OB/GYN prescribes an antidepressant, the system automatically alerts the patient’s psychiatrist. Over 1,200 U.S. hospitals now use it. The NIH is launching a major study in late 2024 called PACT, tracking 5,000 pregnancies with genetic testing to predict which meds work best for each woman. This isn’t sci-fi-it’s the next step toward truly personalized care.What You Can Do Today
You don’t need to wait for the system to fix itself. Here’s your action plan:- If you’re pregnant or planning to be, ask your OB/GYN: “Do you work with a psychiatrist for medication management?”
- If they say no, ask for a referral to a maternal mental health specialist.
- Bring a printed list of your current meds, dosages, and mental health history to your next appointment.
- Request a joint consultation if you’re on mood stabilizers, have a history of psychosis, or your symptoms are worsening.
- Use ACOG’s Reproductive Safety Checklist to track risks side-by-side.
- Keep a simple log: date, mood score (1-10), meds taken, any side effects.
Final Thought: Your Mental Health Is Part of Your Pregnancy Care
Pregnancy isn’t just about ultrasounds and prenatal vitamins. It’s about the whole person-the mind included. Treating depression or anxiety isn’t overmedicating. It’s protecting your ability to bond with your baby, to sleep, to eat, to get through the day. The best care doesn’t choose between you and your baby. It chooses both.Can I take antidepressants while breastfeeding?
Yes, many antidepressants are safe during breastfeeding. Sertraline and escitalopram are the most recommended because they transfer in very low amounts to breast milk-often lower than what your baby was exposed to during pregnancy. Studies show no increased risk of developmental delays or behavioral issues in babies exposed to these medications through breast milk. Always confirm with your psychiatrist and OB/GYN before starting or changing any medication.
What if my OB/GYN and psychiatrist give me different advice?
Don’t choose sides-ask for a joint meeting. Conflicting advice is a sign that coordination is missing, not that one provider is wrong. Request that both providers sit down together (in person or via video) to review your case. Bring your medication list, symptoms, and any research you’ve done. ACOG’s Reproductive Safety Checklist can help turn opinions into shared decisions based on data.
Is it safe to stay on mood stabilizers during pregnancy?
It depends on the medication. Lithium can be used with close monitoring of blood levels and fetal heart rate. Valproate is strictly avoided-it carries a 10.7% risk of major birth defects. If you have bipolar disorder, stopping your meds without a plan increases your risk of relapse by up to 70%. Work with both your OB/GYN and psychiatrist to find the safest option and monitor you closely throughout pregnancy.
Why does my dose need to change during pregnancy?
Your body changes a lot during pregnancy. Blood volume increases by 40-50%, your kidneys filter drugs faster, and liver enzymes become more active-especially in the third trimester. This means many medications clear from your system quicker, which can lower their effectiveness. A dose that worked before pregnancy may no longer be enough. Regular check-ins every 4 weeks help adjust doses before symptoms return.
How do I know if I need a psychiatrist involved at all?
If you’ve been diagnosed with depression, anxiety, bipolar disorder, or PTSD-and you’re taking medication-you need a psychiatrist involved. Even if your OB/GYN prescribes the meds, they’re not trained to manage complex psychiatric conditions. ACOG recommends psychiatrist collaboration for any case involving bipolar disorder, treatment-resistant depression, or past hospitalizations. If you’re unsure, ask: “Would you feel comfortable managing this alone if I had a relapse?” If the answer isn’t a confident yes, get a specialist involved.


14 Comments
Doreen PachificusJanuary 3, 2026 AT 23:33
My OB/GYN just shrugged when I asked about sertraline during breastfeeding. Said 'it's probably fine' and moved on. Felt like I was asking if it was okay to eat sushi.
Enrique GonzálezJanuary 5, 2026 AT 03:35
This is the kind of info I wish I had before my third trimester. So many women are left guessing. Seriously, this should be mandatory reading for every OB/GYN office.
Ethan PurserJanuary 5, 2026 AT 09:18
They say 'coordination is essential' like it's some noble ideal... but in reality? Your OB/GYN is overworked, your psychiatrist is on a 3-month waitlist, and your insurance won't cover a joint visit unless you're actively suicidal. We're told to 'advocate for ourselves' like it's a personality trait, not a full-time job. And then we're shamed for not being 'proactive enough.'
It's not about being lazy. It's about being trapped in a system designed to fail women who need help. The checklist is nice. The data is solid. But none of it matters if your provider doesn't have time to open a second tab, let alone a second chart.
I stopped taking my meds because I was too tired to fight. And now I'm here, typing this at 3 a.m. while my baby screams, wondering if I made the right choice. Spoiler: I didn't. But I was exhausted. And nobody asked if I was okay. They just asked if I'd taken my pills.
Cassie TynanJanuary 6, 2026 AT 10:47
Oh wow, so now we're supposed to be our own case managers? Great. I'm sure my 40-hour work week and toddler tantrums are just the perfect setup for coordinating between two specialists who don't talk to each other. And let's not forget the 14-day insurance delay. By the time I get an appointment, my baby will be in college.
Meanwhile, my OB/GYN still thinks 'natural remedies' like 'walking in nature' are a substitute for SSRIs. I'm not a Pinterest board. I'm a human with a brain that's actively trying to shut down. Can we stop pretending this is about wellness and start admitting it's about access?
Rory CorriganJanuary 8, 2026 AT 09:48
sertraline = good
paroxetine = bad
valproate = nope
lithium = maybe
tl;dr: take the one that doesn't turn your baby into a science experiment. also, ask for a joint meeting. or just yell into the void. same result.
Stephen CraigJanuary 9, 2026 AT 22:55
Clear guidelines exist. Implementation is broken. Systemic failure, not individual negligence.
Jack WernetJanuary 10, 2026 AT 20:19
As a clinician who has worked in maternal mental health for over a decade, I can confirm that the data presented here is not only accurate but underrepresented in clinical practice. The disconnect between obstetric and psychiatric care remains one of the most persistent and dangerous gaps in women's healthcare. While institutional frameworks like Epic's Perinatal Module are promising, they are not yet ubiquitous. The onus still falls disproportionately on the patient to navigate this labyrinth. I urge all providers-regardless of specialty-to institutionalize routine communication protocols, not as an add-on, but as a core standard of care. The Reproductive Safety Checklist is not a suggestion; it is a clinical imperative.
Roshan AryalJanuary 12, 2026 AT 12:40
You Americans think your healthcare system is advanced? Ha. In India, we don't have psychiatrists who talk to OB/GYNs because we don't have psychiatrists at all outside big cities. Women here either take nothing or go to a pharmacy and buy whatever the pharmacist recommends. Your '0.5% risk' is a luxury. We're lucky if the baby survives the birth. Stop acting like your checklist is a revolution. It's just a Band-Aid on a hemorrhage.
en MaxJanuary 14, 2026 AT 03:01
It is imperative to underscore that the integration of psychiatric and obstetric care pathways, when executed with fidelity to evidence-based protocols, significantly mitigates perinatal morbidity and mortality. The utilization of standardized tools such as the ACOG Reproductive Safety Checklist facilitates transdisciplinary alignment and reduces clinical ambiguity. Furthermore, the implementation of interoperable EHR systems, such as Epic’s Perinatal Mental Health Module, constitutes a critical infrastructure advancement that enables longitudinal, patient-centered care coordination. Clinicians are ethically obligated to prioritize such frameworks, particularly in cases involving mood stabilizers or treatment-resistant conditions, wherein the risk-benefit calculus is non-trivial and requires multidisciplinary consensus.
Angie ReheJanuary 14, 2026 AT 13:28
Why are we still letting OB/GYNs prescribe antidepressants? They’re not trained for this! I had a patient last week who was on 150mg sertraline because her OB ‘read a blog post.’ Her psychiatrist didn’t know until she crashed. That’s malpractice. And now you want me to believe a checklist fixes this? No. We need mandatory joint certification. No OB should prescribe psychiatric meds unless they’ve co-signed a treatment plan with a psychiatrist. And if your EHR doesn’t auto-alert the other provider? You’re not just behind-you’re dangerous.
Jay TejadaJanuary 15, 2026 AT 06:03
bro i just wanted to nap after my baby was born and now i have to be a medical coordinator? lol. i took sertraline. baby is fine. i’m fine. if your docs don’t talk, call them together. problem solved. stop overcomplicating it. also, stop crying about insurance. just get the meds. they’re not magic. they’re medicine.
Shanna SungJanuary 16, 2026 AT 04:51
They’re hiding something. Why does the FDA only update labels after 15,000 cases? Why did they wait until 2024 to say sertraline needs dose adjustments? And why is the NIH launching a study on genetics but no one’s asking why Big Pharma funded the original studies? This isn’t science-it’s a cover-up. They don’t want you to know that SSRIs can cause autism. They just want you to take the pill and shut up.
Brendan F. CochranJanuary 16, 2026 AT 14:55
obgyns are just scared of lawsuits so they tell you to stop your meds. psychiatrists are scared of losing patients so they say keep going. nobody wants to be responsible. so you get stuck in the middle like a damn sandwich. just take the damn sertraline. my cousin did it and her kid is now a pro soccer player. if you're scared, go to a different doc. problem solved. stop overthinking it.
jigisha PatelJanuary 16, 2026 AT 16:42
The assertion that sertraline poses only a 0.5% absolute risk increase for cardiac defects is statistically misleading. The baseline population risk is not adequately contextualized within socioeconomic subgroups. Furthermore, the British Association for Psychopharmacology’s recommendation for monotherapy ignores pharmacogenetic variability. A 30% reduction in neonatal complications is not clinically significant when the sample population is predominantly Caucasian and middle-class. The NIH’s PACT study will likely replicate these biases. Until pharmacogenomic screening is mandated for all pregnant women on psychiatric medication, these guidelines remain ethically incomplete and culturally colonial.