OIC Treatment Suitability Checker
This tool helps you and your healthcare provider determine if PAMORAs may be appropriate for your opioid-induced constipation (OIC). Based on the article, PAMORAs are only recommended when first-line laxatives don't work and may not be suitable for everyone due to contraindications.
When you start taking opioids for chronic pain, you’re likely focused on relief - not the side effects. But for 40 to 60% of people on long-term opioids, constipation isn’t just a nuisance. It’s a persistent, often debilitating problem that doesn’t go away with time. Unlike nausea or drowsiness, which may fade as your body adjusts, opioid-induced constipation (OIC) sticks around as long as you’re on the medication. And if left unchecked, it can lead to nausea, bloating, vomiting, and even dangerous bowel obstructions.
Why Opioids Cause Constipation
Opioids don’t just block pain signals in the brain. They also latch onto receptors in your gut, specifically the μ-opioid receptors in the intestinal wall. This slows down the natural muscle contractions that push food and waste through your digestive tract. The result? Sluggish movement, extra water absorption, harder stools, and tighter anal sphincters that make it harder to pass them. It’s not just about being ‘regular’ - it’s about your body’s ability to function normally.Many patients assume constipation will improve after a few days. It won’t. In fact, studies show that once OIC starts, it rarely resolves on its own. Even if you’ve been on opioids for months, your bowel habits can keep getting worse. That’s why waiting until you’re struggling to poop is a mistake.
Prevention Starts on Day One
The most effective way to handle OIC isn’t to treat it after it happens - it’s to prevent it from the moment you start your opioid therapy. Experts agree: if you’re prescribed opioids for more than a few days, you should also start a laxative the same day.Research from Johns Hopkins shows that proactive laxative use prevents 60-70% of severe OIC cases. Yet, in primary care settings, only about 32% of patients get this advice. In palliative care, where providers are more familiar with the issue, the rate jumps to 85%. That gap isn’t due to lack of evidence - it’s due to missed opportunities.
Pharmacists play a key role here. When they proactively recommend laxatives during opioid dispensing, initiation rates increase by 43%. That’s a huge difference. Don’t wait for your doctor to mention it. Ask: “Should I be taking something for constipation with this?”
First-Line Treatments: What Actually Works
Not all laxatives are created equal when it comes to OIC. Traditional options like stool softeners (docusate) often fail because they don’t address the underlying nerve slowdown. Instead, two types of laxatives have proven more effective:- Osmotic laxatives - Polyethylene glycol (PEG 3350, like Miralax) draws water into the colon, softening stool and encouraging movement. It’s gentle, safe for long-term use, and doesn’t cause dependency.
- Stimulant laxatives - Senna or bisacodyl trigger muscle contractions in the intestines. These work faster than osmotic agents but shouldn’t be used daily for more than a week without medical supervision.
Many patients start with one or both of these. But here’s the catch: up to 68% of people still report inadequate relief. That’s because OIC is mechanistically different from regular constipation. Your gut isn’t just dry - it’s paralyzed by opioids.
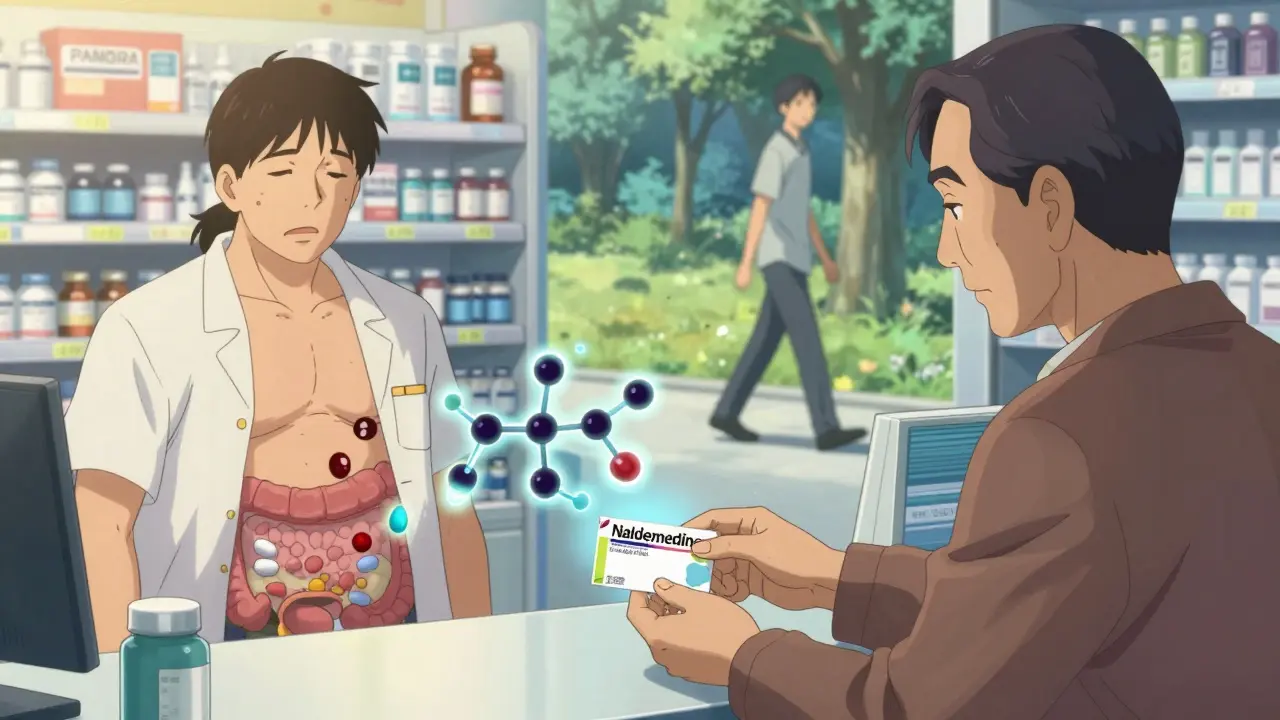
When Laxatives Aren’t Enough: PAMORAs
If you’re still struggling after trying osmotic and stimulant laxatives, it’s time to consider a different class of drugs: peripherally acting μ-opioid receptor antagonists, or PAMORAs. These are the only medications designed specifically to reverse the gut effects of opioids without touching pain relief.PAMORAs work by blocking opioid receptors in the intestines - but not in the brain. Because they can’t cross the blood-brain barrier easily, your pain control stays intact while your bowels start moving again.
There are four FDA-approved PAMORAs for OIC:
- Methylnaltrexone (Relistor®) - Given as a subcutaneous injection, it works within 30 minutes. Often used in advanced illness or palliative care. A new once-weekly formulation is now available.
- Naldemedine (Symproic®) - An oral pill taken daily. Approved for adults with chronic noncancer pain and cancer patients. Studies show it also reduces opioid-induced nausea.
- Naloxegol (Movantik®) - An oral tablet taken daily. Works well for chronic noncancer pain.
- Lubiprostone (Amitiza®) - Not technically a PAMORA, but works differently by activating chloride channels in the gut to increase fluid secretion. FDA-approved for women, though effective in men too.
Patients on Reddit and PatientsLikeMe report dramatic improvements: “Relistor worked when nothing else did,” or “Naldemedine let me stay on my pain meds without constant bathroom struggles.” But it’s not perfect. About 28% report abdominal cramping. And cost is a major barrier - these drugs can run $500 to $900 a month without insurance.
Who Should Avoid PAMORAs
PAMORAs are powerful, but not for everyone. They’re contraindicated if you have a known or suspected bowel obstruction, recent abdominal surgery, or active inflammatory bowel disease like Crohn’s or ulcerative colitis. In rare cases, the increased bowel movement can cause perforation - a life-threatening tear in the intestinal wall.Patients with a history of GI surgery, radiation to the abdomen, or severe diverticulosis need extra caution. Your doctor should assess your risk before prescribing. If you suddenly develop sharp abdominal pain, fever, or vomiting while on a PAMORA, seek emergency care immediately.
Real-World Barriers to Treatment
Even with proven options, OIC remains undertreated. Why? Three big reasons:- Patient reluctance - Many don’t want to take “another pill.” They think constipation is just part of the deal.
- Underdosing - Taking one Miralax packet a day won’t cut it. Most need two or more, plus stimulants.
- Insurance hurdles - Medicare Part D plans require prior authorization for 41% of PAMORAs. Commercial insurers often force patients to try cheaper laxatives first, even when guidelines say they’re ineffective.
A 2023 survey found that 57% of patients stopped PAMORAs within six months due to cost or lack of results. That’s tragic - because for many, these drugs are life-changing.

What’s Next: The Future of OIC Care
The global OIC treatment market is growing fast - projected to hit $2.1 billion by 2027. New developments are on the horizon:- Combination therapies - pills that pair low-dose PAMORAs with osmotic agents for better results.
- Personalized treatment - research is underway to identify genetic markers that predict who responds best to which drug.
- Guideline updates - ASCO now recommends naldemedine for cancer patients starting opioids, citing improved quality of life and reduced nausea.
By 2026, experts predict we’ll see treatment plans tailored to individual biology, not just trial and error.
How to Monitor Your Progress
Don’t guess whether your treatment is working. Use a simple tool called the Bowel Function Index (BFI). It’s a three-question survey that scores constipation severity from 0 to 100. A score above 30 means you need to adjust your plan.Track your bowel movements daily. Note:
- How many times you had a bowel movement
- Stool consistency (use the Bristol Stool Scale - types 3 and 4 are ideal)
- Straining, feeling of incomplete emptying, or bloating
Bring this log to your next appointment. It gives your doctor real data - not just “I feel constipated.”
Bottom Line: You Don’t Have to Suffer
Opioid-induced constipation isn’t inevitable. It’s treatable - but only if you act early and know your options. Start laxatives on day one. Don’t wait for symptoms. If they don’t work after a couple of weeks, ask about PAMORAs. Advocate for yourself. Insurance may push back, but your quality of life matters more.There are over 73 million Americans on long-term opioids for pain. You’re not alone. And you don’t have to live with constipation as the price of pain relief.
Can opioid-induced constipation go away on its own?
No. Unlike other opioid side effects like drowsiness or nausea, which often improve over time, opioid-induced constipation (OIC) persists as long as you’re taking opioids. It doesn’t resolve without intervention because opioids directly slow gut motility - a mechanism that doesn’t adapt with continued use.
Are over-the-counter laxatives effective for OIC?
They help some people, but not enough. Osmotic laxatives like polyethylene glycol (Miralax) and stimulant laxatives like senna are recommended as first-line treatments, but studies show up to 68% of patients still experience inadequate relief. OIC is mechanistically different from regular constipation, so standard laxatives often fall short.
What are PAMORAs and how do they work?
PAMORAs (peripherally acting μ-opioid receptor antagonists) are drugs like naldemedine, methylnaltrexone, and naloxegol. They block opioid receptors in the gut, reversing constipation without affecting pain relief in the brain. Because they don’t cross the blood-brain barrier well, your pain control stays intact while your bowels start moving normally again.
Is naldemedine better than other PAMORAs?
For cancer patients starting opioids, naldemedine is the preferred choice according to 2024 ASCO guidelines - it not only improves bowel function but also reduces opioid-induced nausea and vomiting. For noncancer chronic pain, naloxegol and methylnaltrexone are equally effective. The best option depends on your condition, delivery preference (pill vs. injection), and insurance coverage.
Can PAMORAs cause serious side effects?
Yes. The biggest risk is gastrointestinal perforation - a tear in the bowel wall - especially in patients with prior abdominal surgery, inflammatory bowel disease, or bowel obstructions. Other common side effects include abdominal pain, diarrhea, and nausea. These drugs carry FDA-mandated black box warnings and require careful patient selection.
Why is OIC often under-treated?
Patients often don’t report it, assuming it’s normal. Doctors may overlook it or assume laxatives are enough. Insurance frequently blocks access to PAMORAs due to cost, requiring prior authorization or step therapy. Only 32% of primary care providers start laxatives at opioid initiation, compared to 85% in palliative care.
How can I talk to my doctor about OIC treatment?
Be direct: “I’m on opioids and having trouble with constipation. I’ve tried Miralax and senna, but it’s not working well. Can we discuss PAMORAs like naldemedine or methylnaltrexone?” Bring a bowel log showing frequency, stool type, and symptoms. Ask about insurance coverage and whether your plan requires prior authorization.
Are there non-medication ways to manage OIC?
Yes - but they’re not enough alone. Drink plenty of water (at least 8 cups daily), eat fiber-rich foods like oats, beans, and vegetables, and move regularly - even short walks help. Avoid delaying bowel movements. However, because opioids directly paralyze gut nerves, lifestyle changes alone rarely resolve OIC. They should support, not replace, medical treatment.
How long does it take for PAMORAs to work?
It varies. Methylnaltrexone injections work within 30 minutes. Oral PAMORAs like naldemedine and naloxegol usually produce a bowel movement within 24 to 48 hours. Lubiprostone may take 1-2 days. Consistency matters - these are daily treatments, not one-time fixes.
Is OIC more common in older adults?
Yes. Older adults are at higher risk due to slower gut motility, reduced physical activity, and more frequent use of multiple medications that worsen constipation. Studies show OIC affects up to 70-100% of hospitalized cancer patients over 65. Prevention and early intervention are even more critical in this group.


10 Comments
Vinayak NaikJanuary 5, 2026 AT 21:00
Bro this is gold. Opioids hit my pops hard after his back surgery - he was stuck like a turtle on its shell. Tried Miralax, senna, even prunes like a grandpa from 1987. Nothing. Then we found naldemedine. First day? He pooped like a man reborn. Cost? Yeah, it’s a beast. But hey, when you’re not vomiting from bloating and can actually sit through dinner without crying, you learn to fight the insurance gods.
Cam JaneJanuary 7, 2026 AT 16:30
Thank you for writing this. I’ve been on opioids for 7 years after my accident. No one ever told me to start laxatives day one. I thought I was just ‘slow.’ I didn’t know it was fixable. I wish I’d known this sooner. You just made my life easier. Seriously. Thank you.
Wesley PereiraJanuary 9, 2026 AT 12:15
So let me get this straight - we’ve got a $900/month drug that fixes what a $5 bottle of Miralax can’t… but insurance makes you jump through 12 hoops first? Classic American healthcare. You’re not sick, you’re just inconvenient. Meanwhile, my doc still thinks ‘drink more water’ is a treatment plan. Bro, my gut’s got the mobility of a fax machine.
Tom SwintonJanuary 10, 2026 AT 01:35
Man, I’ve seen this play out in my clinic for years - patients on opioids for years, never asked about constipation until they’re in ER with a bowel obstruction. And the worst part? They’re ashamed to bring it up. Like it’s embarrassing. But here’s the truth: your gut doesn’t care if you’re tough. It’s just a tube with nerves. Opioids turn it into a graveyard. And if you’re not proactive? You’re not just ‘constipated’ - you’re one step away from a perforation. Start PEG 3350 on day one. Don’t wait. Don’t hope. Don’t assume. Just do it. And if your doctor says ‘try fiber first’ - ask them if they’ve ever had to clean up a 72-year-old’s colostomy bag after a failed bowel resection. Because I have. And I’ll never let a patient wait again.
Stuart ShieldJanuary 10, 2026 AT 09:43
This is the kind of thing that makes me believe in humanity again. I’m in London, and my mum’s on long-term opioids for arthritis. We stumbled onto Relistor after six months of misery. She cried when she could finally go without screaming. The cost? We paid out of pocket. Worth every penny. The fact that someone took the time to write this - not just for doctors, but for the people who feel broken - that’s real. Thank you.
Pavan VoraJanuary 10, 2026 AT 16:35
From India, I’ve seen so many elderly patients suffer silently - no one talks about this. Even doctors here think it’s ‘normal aging.’ But your post? It’s like a flashlight in a dark room. I shared it with my uncle’s oncologist. He didn’t know about naldemedine. Now he’s prescribing it. Small change, but it matters. Thank you for making this real.
Dana TerminiJanuary 11, 2026 AT 13:35
Just wanted to say: if you’re reading this and you’re on opioids - please, please, please talk to your pharmacist. They’re the unsung heroes here. I asked mine about constipation when I got my first script. She handed me Miralax and a printed guide. No judgment. Just help. That’s the kind of care we need more of.
Gabrielle PanchevJanuary 12, 2026 AT 15:27
Wait - so you’re telling me we’ve got a drug that blocks opioid receptors in the gut but not the brain? That’s like having a bouncer who only kicks out the troublemakers at the club, not the VIPs. Sounds too good to be true. What’s the catch? Are we just trading constipation for diarrhea and cramps? And why isn’t this in every pain clinic? Something smells off.
Amy LeJanuary 12, 2026 AT 20:59
They want you to believe this is a medical breakthrough. But let’s be real - Big Pharma made a billion-dollar product out of a side effect they created. Opioids were never meant to be long-term. Now they’re selling us $900 pills to fix the damage. Classic. You’re not healing. You’re just paying to keep the machine running.
Melanie ClarkJanuary 13, 2026 AT 22:00
Just wait till the government starts tracking your bowel movements. Next thing you know, your insurance will deny your opioid script if your Bristol score is below 3.5. They’ll call it ‘non-compliance.’ They’ll force you to walk 10K steps a day or lose your pain meds. This is how they control us. They don’t care if you’re in pain. They care if you’re ‘productive.’