Digoxin-Amiodarone Dose Calculator
Why This Matters
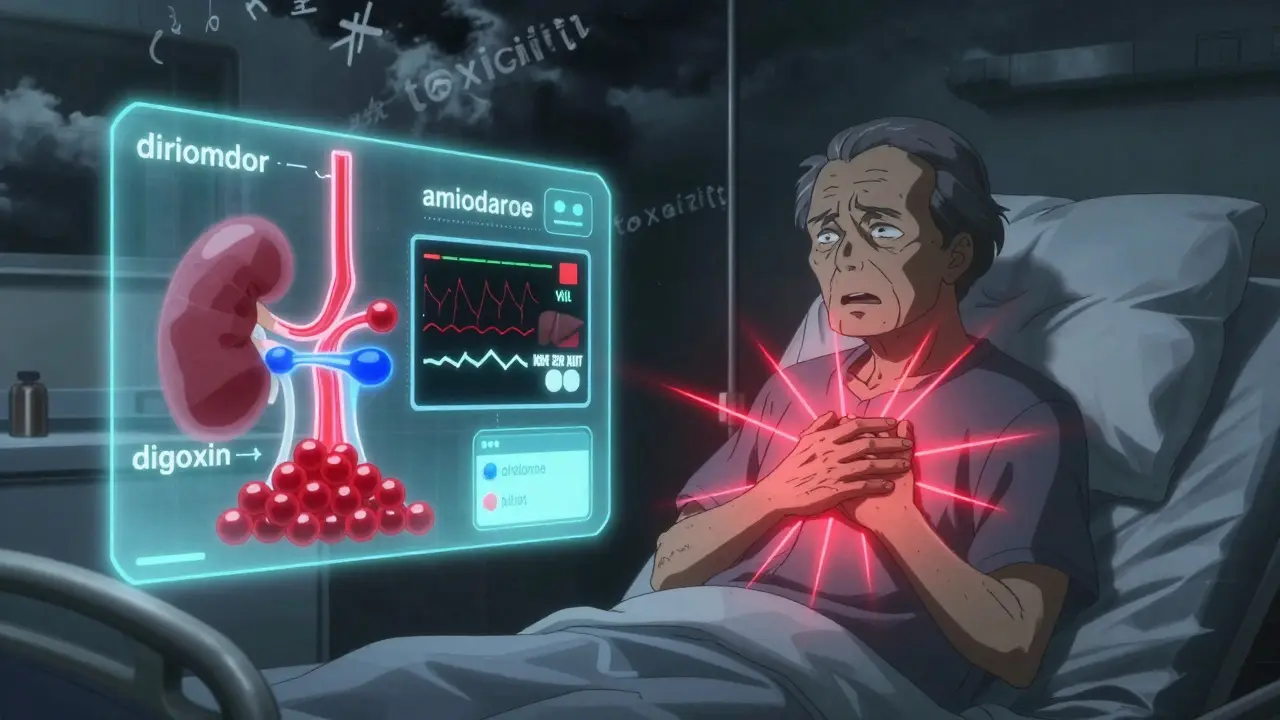
Digoxin has a narrow therapeutic window (0.5-0.9 ng/mL). When combined with amiodarone, digoxin levels can double. Always reduce the digoxin dose immediately when starting amiodarone.
Warning: The interaction happens rapidly. Delaying dose adjustment increases the risk of severe toxicity including cardiac arrest, stroke, or death.
Adjust Digoxin Dose for Amiodarone
Why This Drug Combo Can Kill You
Imagine you’re on digoxin to control your heart rhythm. You’ve been stable for months. Then your doctor adds amiodarone because your atrial fibrillation got worse. Everything seems fine-until you start feeling nauseous, your vision gets blurry, and your heart slows down dangerously. You end up in the ICU. This isn’t rare. It happens because digoxin and amiodarone don’t just interact-they amplify each other’s dangers in a way that can be fatal if not handled correctly.
Digoxin is a heart medication with a razor-thin safety margin. The difference between a therapeutic dose and a toxic one is tiny: 0.5 to 0.9 nanograms per milliliter in your blood. Go above that, and you risk vomiting, confusion, dangerous heart rhythms, or even death. Amiodarone, used for serious arrhythmias, doesn’t just add to the risk-it multiplies it. When taken together, digoxin levels can jump by 100% or more. That’s not a small bump. That’s a trip from safe to lethal.
How Amiodarone Turns Digoxin Into a Time Bomb
It’s not magic. It’s biology. Amiodarone blocks a protein called P-glycoprotein, which normally helps your body flush digoxin out through your kidneys and liver. When that gatekeeper is shut down, digoxin builds up like traffic on a highway with no exits. Studies show digoxin’s clearance drops by nearly 30%. Its half-life stretches from about two days to over three. That means even if you take the same dose, your body holds onto twice as much.
And it’s not just amiodarone itself. Its metabolite, desethylamiodarone, sticks around for months after you stop taking it. So even if you quit amiodarone, your digoxin levels can stay dangerously high for 60 days or longer. This isn’t a short-term problem. It’s a long-term ticking clock.
The Numbers Don’t Lie: Real-World Consequences
A 2021 study in Circulation: Arrhythmia and Electrophysiology found patients on both drugs were 2.3 times more likely to be hospitalized for digoxin toxicity than those on other common combos like digoxin and furosemide. In one 2021 analysis, patients who kept their full digoxin dose when starting amiodarone had a 27% higher chance of dying within 30 days. That’s not a risk. That’s a tragedy waiting to happen.
And it’s not just theory. A 2023 case report described a 72-year-old woman who developed a potassium level of 6.8 mEq/L-life-threateningly high-and a dangerously slow heart rate after starting amiodarone at her usual digoxin dose. She needed four days in the ICU. She survived. Many don’t.
Even worse, a 2024 study showed this combo increased stroke risk by more than double. Why? High digoxin levels may make blood more likely to clot. Add that to the fact that many patients on these drugs are elderly, have kidney problems, or are on other medications-and you’ve got a perfect storm.
What Doctors Should Do (But Often Don’t)
Guidelines have been clear for decades. When you start amiodarone in someone already on digoxin, cut the digoxin dose in half. Right away. Don’t wait for blood tests. Don’t wait to see symptoms. Do it before the first pill of amiodarone hits the system.
For patients with kidney issues-creatinine clearance under 50 mL/min-drop it even further, to one-third of the original dose. That’s not a suggestion. That’s a standard of care. The 2022 European Heart Rhythm Association guide and the 2023 ASHP guidelines both say this. So why do so many patients still get the wrong dose?
A 2022 study across 15 U.S. hospitals found only 44% of patients had their digoxin dose reduced properly when amiodarone was added. In community hospitals, it was worse-68% of cases missed the mark. That’s not a mistake. That’s a systemic failure.
How to Get It Right: A Step-by-Step Plan
- Check digoxin level before starting amiodarone. Write it down. This is your baseline.
- Reduce digoxin by 50% the day you start amiodarone. Even if the level is low. Even if the patient feels fine. This isn’t optional.
- Recheck the digoxin level 72 hours after starting amiodarone. Levels peak around 1-2 weeks, but the first major shift happens in 3 days.
- For kidney-impaired patients, check levels again at 24, 72, and 168 hours. Their bodies clear digoxin slower. They need tighter monitoring.
- Watch for symptoms: Nausea, vomiting, yellow or green halos around lights, dizziness, slow pulse, or confusion. These aren’t side effects-they’re warning signs.
- Keep checking levels for months after stopping amiodarone. Because the metabolite lingers, toxicity can show up weeks later.
One hospital system in Michigan cut digoxin toxicity from 12% to 2% in a year by making this protocol mandatory. They didn’t change drugs. They didn’t buy new tech. They just followed the rules.
What About Alternatives?
Here’s the hard truth: digoxin isn’t the best choice for most people with atrial fibrillation anymore. Beta-blockers like metoprolol or calcium channel blockers like diltiazem are safer, more predictable, and don’t have deadly interactions with amiodarone.
The 2024 European Society of Cardiology draft guidelines now recommend these as first-line for rate control-especially if amiodarone is likely to be used. Digoxin should be reserved for patients who can’t tolerate those drugs, or those with heart failure who still benefit from its inotropic effect.
And even then, if amiodarone is needed, the dose reduction rule still applies. No exceptions.
The Bigger Picture: Why This Keeps Happening
This interaction isn’t new. It’s been known since the 1980s. Yet it still kills people. Why?
Because it’s invisible. You don’t see the P-glycoprotein blockade. You don’t feel the digoxin building up. By the time symptoms show, it’s often too late. Many clinicians think, “She’s been on digoxin for years-she’s fine.” But fine yesterday doesn’t mean safe today.
Electronic health record alerts help. The Veterans Health Administration cut toxicity events by 41% after adding automated warnings when both drugs are prescribed. But alerts aren’t enough. They need to be mandatory, not optional. And they need to be paired with education.
Pharmacists who intervened directly in patient care reduced inappropriate dosing from 58% to 12%. That’s not magic. That’s accountability.
Final Reality Check
There are about 1.2 million Americans on both digoxin and amiodarone right now. That’s more than the population of Birmingham, where I live. And every single one of them is at risk.
This isn’t about being perfect. It’s about being consistent. Cut the dose. Monitor early. Watch for symptoms. Choose safer alternatives when you can. If you’re managing a patient on both drugs and you haven’t reduced the digoxin, you’re not just being cautious-you’re being reckless.
The science is clear. The guidelines are clear. The data is clear. What’s left is action.
What is the safe digoxin level when taking amiodarone?
The therapeutic range for digoxin is still 0.5-0.9 ng/mL, even when taking amiodarone. But because amiodarone raises digoxin levels by up to 100%, you must reduce the digoxin dose upfront to stay within that range. Never assume a pre-amiodarone level is safe after starting amiodarone.
How soon after starting amiodarone should I check digoxin levels?
Check digoxin levels 72 hours after starting amiodarone. Levels begin rising within days, peak around 1-2 weeks, and can stay high for months. Waiting longer risks missing the window to prevent toxicity.
Can I just lower the digoxin dose gradually instead of cutting it in half right away?
No. The interaction happens fast. Delaying the dose reduction increases the risk of toxicity before you even see symptoms. Studies show the biggest spike in digoxin levels occurs within the first 3-7 days. Immediate 50% reduction is the only safe approach.
Does this interaction happen with dronedarone too?
Yes. Dronedarone, a related drug, also increases digoxin levels. The PALLAS trial showed a 31% higher risk of cardiovascular death when dronedarone was added to digoxin. The same dose-reduction rules apply.
Why is digoxin still used if it’s so dangerous with amiodarone?
Digoxin still has a role in heart failure with reduced ejection fraction, especially when beta-blockers or other agents aren’t enough. It’s not the first choice for atrial fibrillation anymore, but in specific cases, its benefits outweigh the risks-if managed correctly. The danger isn’t digoxin itself. It’s the failure to adjust for interactions.
What symptoms should I watch for in a patient on both drugs?
Look for nausea, vomiting, loss of appetite, blurred or yellow/green vision, dizziness, confusion, and an unusually slow or irregular pulse. These are classic signs of digoxin toxicity. If seen, stop the drug, check the level, and get help immediately.
How long does the interaction last after stopping amiodarone?
Amiodarone and its active metabolite can stay in your system for up to 60 days after the last dose. Digoxin levels may remain elevated during this time. Never assume the interaction is over just because amiodarone was stopped. Continue monitoring digoxin levels for at least two months.
Are there any blood tests I should do besides digoxin levels?
Yes. Check potassium, magnesium, and kidney function (creatinine, eGFR). Low potassium or magnesium makes digoxin toxicity more likely. Poor kidney function slows digoxin clearance. These factors compound the risk. Don’t treat digoxin in isolation.
What to Do Next
If you’re prescribing or managing these drugs, start today. Review every patient on digoxin. Ask: Are they on amiodarone? Are they on any other drug that might affect P-glycoprotein? If yes, reduce the digoxin dose now. Set a reminder to check levels in 72 hours. Talk to the pharmacist. Use the EHR alert if your hospital has one.
If you’re a patient on both drugs and you’ve never had your dose adjusted-ask your doctor why. Don’t wait for symptoms. This interaction doesn’t announce itself. It sneaks up. And when it hits, it hits hard.
The science is settled. The protocol is simple. The cost of inaction? Too high to ignore.

14 Comments
lisa BajramJanuary 10, 2026 AT 00:48
I work in cardiology and this is STILL a nightmare. I had a patient last month who came in with digoxin toxicity after starting amiodarone-no dose adjustment. She was confused, had visual halos, and her heart rate was 38. We had to pull her off both drugs. It’s 2025. Why is this still happening?Every single time I see this combo, I reduce digoxin by 50% before the first amiodarone pill. No exceptions. No ‘let’s wait and see.’ The data is screaming. Listen to it.
Jaqueline santos bauJanuary 10, 2026 AT 12:29
I can’t believe people still use digoxin. Like, really? It’s basically poison with a heartbeat. Amiodarone is already a walking chemical bomb, and now you’re mixing it with a loaded gun? Someone’s gonna die. And when they do, it’ll be because someone thought ‘she’s been fine for years’ was a medical strategy. Wake up.Kunal MajumderJanuary 10, 2026 AT 15:06
In India, we see this a lot. Elderly patients on digoxin for AFib, then get amiodarone because they can’t afford the newer drugs. No one reduces the dose. No one checks levels. We just hope for the best. This post is a wake-up call. I’m sharing it with every resident I train. This isn’t just theory-it’s survival.Aurora MemoJanuary 10, 2026 AT 18:49
I appreciate how clearly this was laid out. The step-by-step plan? Perfect. I’ve seen too many patients slip through the cracks because providers assume ‘if it ain’t broke, don’t fix it.’ But with digoxin and amiodarone, the ‘broken’ part is silent until it’s too late. Thank you for giving us a concrete path forward.chandra tanJanuary 11, 2026 AT 09:50
I’m a pharmacist in Bangalore and we get this combo all the time. Last week, a patient came in with a digoxin level of 3.2 ng/mL-three times the upper limit. He’d been on both drugs for six weeks. No one adjusted. I called the doctor. He said, ‘Oh, I thought the guidelines changed.’ They didn’t. We just forgot. This needs to be in every pharmacy curriculum.Dwayne DicksonJanuary 12, 2026 AT 20:53
The systemic failure described here is not merely negligent-it is a catastrophic abdication of clinical responsibility. The fact that 68% of community hospitals fail to implement this protocol is not an oversight. It is an indictment of a healthcare system that prioritizes convenience over competence. The 27% 30-day mortality increase is not a statistical anomaly. It is a massacre.Ted ConerlyJanuary 13, 2026 AT 01:48
This is one of those things that should be automatic. Like seatbelts. Like fire alarms. If you prescribe amiodarone to someone on digoxin, the EHR should auto-reduce the dose and pop up a warning that won’t go away until you acknowledge it. We’ve got the tech. We’ve got the evidence. We just need the will to use it.Faith EdwardsJanuary 14, 2026 AT 01:33
It is frankly astonishing that such a well-documented, easily preventable, and lethally predictable interaction continues to claim lives. The persistence of this practice suggests a profound intellectual laziness among clinicians who have evidently not read the literature since the 1990s. One must wonder: are they too busy scrolling TikTok to open a journal?Jay AmparoJanuary 15, 2026 AT 14:33
I’ve seen this play out twice in my clinic. Both times, the patients survived because a nurse caught the slow pulse and pushed for a level check. We didn’t have an alert. We didn’t have a protocol. We just had a nurse who cared enough to question it. That’s the real hero here-not the guidelines, not the studies. The people who refuse to look away.Lisa CozadJanuary 16, 2026 AT 05:20
I’m a nurse on a med-surg floor and I’ve seen this too. One guy came in with a digoxin level of 4.1. He was on amiodarone for 8 weeks. His dose was never touched. His family was furious. We had to call the pharmacy team to fix it. I wish we had a checklist. I wish someone had trained us better. This shouldn’t be on us to catch.Saumya Roy ChaudhuriJanuary 16, 2026 AT 10:52
Let me tell you something-this isn’t even the worst interaction. Did you know amiodarone also increases cyclosporine levels by 300%? Or that it can cause thyroid cancer in 20% of long-term users? And you’re worried about digoxin? This is just the tip of the iceberg. If you’re using amiodarone, you’re playing Russian roulette with five bullets. And digoxin is just the first chamber.Ian CheungJanuary 16, 2026 AT 17:32
I’m a med student and this post changed how I think about meds. I used to think drug interactions were just textbook stuff. Now I get it-this isn’t theory. It’s real people vomiting, going blind, dying because someone didn’t hit the button to reduce the dose. I’m printing this out and taping it to my laptop. No more ignoring the obvious.anthony martinezJanuary 17, 2026 AT 00:25
So let me get this straight. We have a drug combo that’s been known to kill since the 80s, guidelines that are crystal clear, and yet we still have a 68% failure rate in community hospitals? That’s not incompetence. That’s institutional malpractice. Someone should be fired. Or sued. Or both.Mario BrosJanuary 17, 2026 AT 13:34
This is why I love being a pharmacist. I get to be the guy who says ‘hold up’ before someone gets hurt. I’ve stopped this combo 17 times this year. Every time, I get a little pushback. ‘But she’s been stable!’ I say: ‘So was the Titanic.’ And then I hand them the protocol. They always thank me later. Don’t wait for the ICU. Do the math. Cut the dose. Save a life.