Race and Medication Efficacy: How Genetics Influence Drug Response
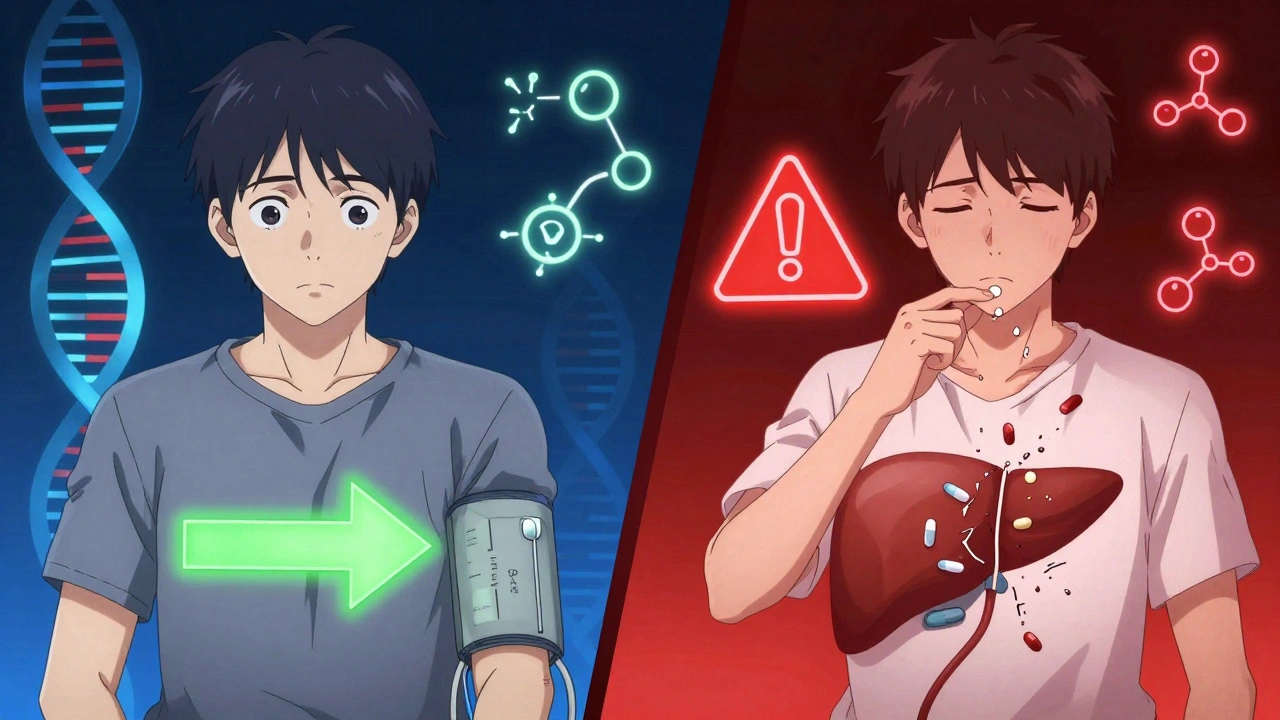
When we talk about race and medication efficacy, how differences in population genetics affect how well drugs work in different groups. Also known as pharmacogenomics, it’s not about stereotypes—it’s about biology. People aren’t treated differently because of their race—they’re treated differently because of their genes, and those genes often cluster in populations shaped by geography, ancestry, and history.
Take warfarin, a blood thinner. Some people need half the dose others do, and that’s not random. Studies show people of African descent often need higher doses than those of European or Asian descent, not because of lifestyle, but because of variants in the CYP2C9 and VKORC1 genes that control how the drug is broken down. Same drug. Same condition. Different biology. This isn’t an exception—it’s the rule. pharmacogenomics, the study of how genes affect drug response explains why a pill that works wonders for one person might do nothing—or cause harm—for another.
And it’s not just warfarin. The heart drug BiDil was approved specifically for Black patients because clinical trials showed it cut death rates by 43% in that group, thanks to a higher frequency of a gene variant affecting nitric oxide response. Beta-blockers like metoprolol work better in white patients than in Black patients for high blood pressure, not because one group is less compliant, but because of differences in how their bodies handle the drug. Even antibiotics like sulfamethoxazole can trigger severe reactions in people with certain G6PD gene variants, which are more common in African, Mediterranean, and Southeast Asian populations.
These aren’t oddities. They’re data points. And they matter. Ignoring them leads to wasted prescriptions, avoidable side effects, and longer hospital stays. The FDA now recommends genetic testing for some drugs before prescribing, and pharmacies are starting to track genetic data to flag risks. But you don’t need a lab test to start paying attention. If a medication doesn’t work for you—or gives you side effects others don’t get—ask: could this be about my genes?
That’s why the posts below cover real-world cases where drug metabolism, safety, and effectiveness hinge on biological differences. From liver disease affecting how drugs break down, to grapefruit changing statin levels, to how acid reducers mess with absorption—each story ties back to one truth: your body processes medicine in its own way. And understanding that isn’t just science—it’s the key to getting the right dose, the right drug, and the right outcome.
Ethnicity influences how your body processes medications due to genetic differences in drug metabolism. Learn how CYP450 enzymes, HLA variants, and pharmacogenomics are changing prescribing practices to improve safety and effectiveness.