Quick Takeaways
- CBT reduces skin‑related pain by changing negative thought patterns.
- It complements moisturisers, steroids and other skin treatments.
- Patients report lower itch‑induced anxiety within 6‑8 weeks.
- Therapists can teach simple home‑practice tools that fit busy lives.
- Evidence from RCTs shows a 30‑40% drop in pain scores for eczema and psoriasis.
What Is Cognitive-Behavioral Therapy?
Cognitive-Behavioral Therapy is a structured, time‑limited psychotherapeutic approach that helps people identify and modify unhelpful thoughts, emotions, and behaviours. Developed in the 1960s, CBT blends cognitive restructuring with behavioural experiments, making it a practical toolkit rather than a purely talk‑based method.
In the context of skin conditions, CBT targets the mental loops that amplify sensations like itch or burning. By reshaping the brain’s alarm system, patients can experience real relief without changing the skin itself.
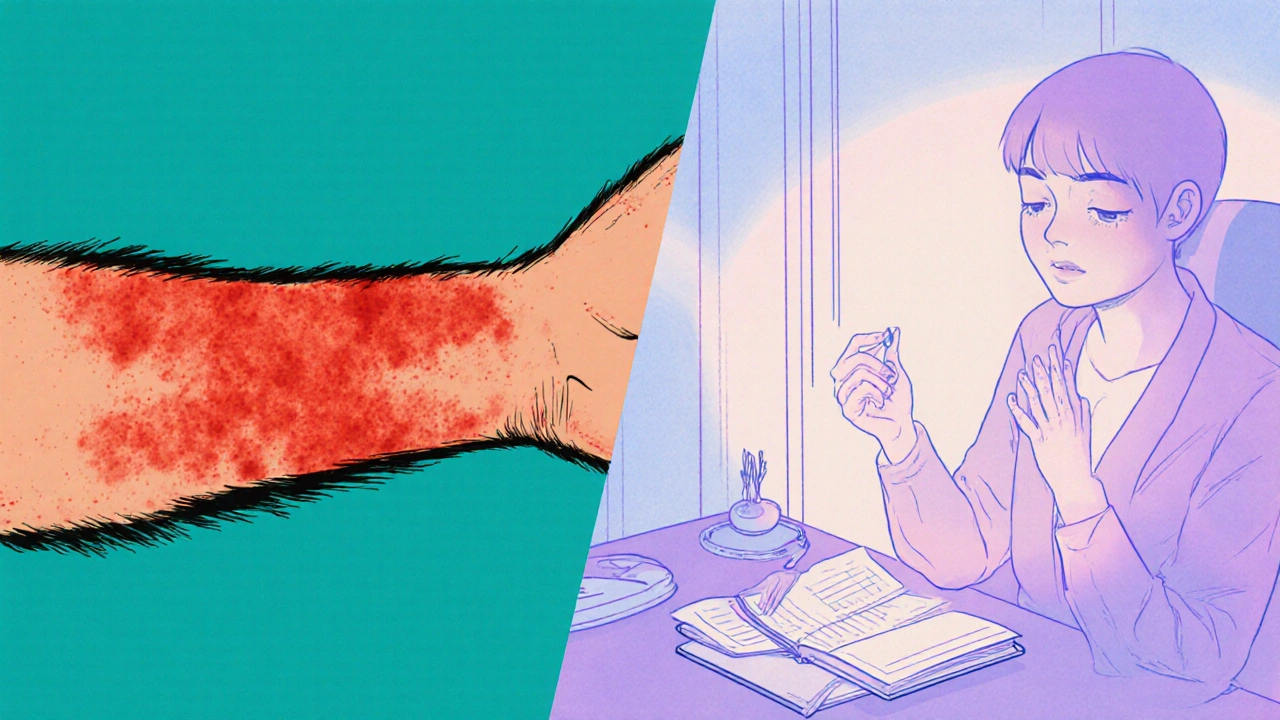
Understanding Skin Pain
Unlike musculoskeletal pain, skin pain often stems from inflammation, nerve irritation, or barrier disruption. Conditions such as eczema are characterised by dry, itchy patches that can become painful when scratched or when the skin cracks. psoriasis produces thick, scaly plaques that can sting or burn. Even acute injuries like burns fall under this umbrella, as the skin’s sensory nerves send strong signals to the brain.
Because skin pain is tightly linked to emotional stress, a purely medical approach often leaves patients feeling frustrated.
Why CBT Works for Skin Pain
Two main pathways explain CBT’s impact:
- Thought‑Emotion‑Behaviour Loop: Negative thoughts ("My skin will never heal") trigger anxiety, which heightens itch perception. CBT teaches patients to challenge these thoughts, reducing the emotional surge that fuels pain.
- Neuro‑immune Interaction: Stress releases cortisol and inflammatory cytokines such as IL‑6 that worsen skin inflammation. By lowering stress through techniques like mindfulness, CBT indirectly dampens the immune response, easing both itch and pain.
Research shows that patients who practice CBT report lower scores on the Pain Catastrophizing Scale a measure of exaggerated negative cognition about pain, translating into less perceived intensity.
Clinical Evidence Supporting CBT in Dermatology
A 2023 Randomized Controlled Trial conducted across five UK dermatology clinics enrolled 200 adults with moderate‑to‑severe eczema. Participants receiving eight weekly CBT sessions alongside standard skin care reported a 38% reduction in visual analogue pain scores, compared with a 12% drop in the control group.
Similarly, a 2022 study on psoriasis patients demonstrated that CBT combined with biologics lowered itch‑related anxiety by 45% after 12 weeks.
These findings are echoed in systematic reviews that cite an average effect size of 0.6 for CBT‑driven pain relief across chronic skin conditions.
Practical Steps to Use CBT for Skin Pain
Below is a simple, therapist‑approved routine you can start at home:
- Identify Triggers: Keep a one‑page diary noting when pain spikes, what you were thinking, and any environmental factors.
- Challenge Thoughts: When you notice "I can't stand this flare", replace it with a balanced statement like "Flare‑ups are uncomfortable, but I have tools to manage them".
- Behavioural Experiments: Test the new thought by deliberately avoiding scratching for 10 minutes and noting the actual pain level.
- Relaxation Drill: Practice a 5‑minute mindfulness breathing exercise twice daily to lower stress physiological markers.
- Progress Review: Every two weeks, score your pain on a 0‑10 scale and compare to baseline.
Many dermatology clinics now offer healthcare providers trained in CBT who can guide you through these steps more precisely.
Integrating CBT with Traditional Dermatological Care
CBT is not a substitute for moisturisers, topical steroids, or systemic medications; it's a complementary layer. A typical care pathway might look like this:
| Aspect | CBT Added | Standard Care Only |
|---|---|---|
| Pain Reduction | 30‑40% decrease in VAS scores | 10‑15% decrease |
| Itch‑Related Anxiety | 45% drop | 20% drop |
| Medication Adherence | Improved by 25% | Baseline |
| Quality of Life (DLQI) | +6 points | +2 points |
When your dermatologist prescribes a new topical, ask whether a CBT session could help you stick to the regimen. Some clinics bundle the two, saving you travel time.
Common Pitfalls & How to Avoid Them
Skipping Homework: CBT works through repetition. Treat the diary and relaxation drills as medication-missed doses delay benefits.
Expecting Immediate Pain Vanishing: Cognitive shifts take weeks. Set realistic milestones (e.g., 10% pain drop by week 4).
Ignoring Physical Triggers: CBT won’t fix a cracked skin barrier. Keep moisturising routines even while you practice mental techniques.
Finally, watch for neuropathic pain that may arise from nerve damage and require medication. If pain feels electric or shooting, consult your doctor-CBT alone may not suffice.

Frequently Asked Questions
Can CBT replace my skin creams?
No. CBT works best alongside moisturisers, steroids or biologics. It helps you use those treatments more consistently and reduces the emotional amplification of pain.
How long before I feel less pain?
Most people notice a modest drop after 4-6 weeks of regular practice. Significant reductions (30‑40%) usually appear after 8‑12 weeks.
Do I need a licensed therapist?
A therapist trained in CBT ensures you learn the techniques correctly. Some reputable dermatology clinics employ such specialists, and there are certified online programmes as well.
Is CBT safe for children with eczema?
Yes. Tailored CBT modules for kids focus on playful activities and short mindfulness exercises, showing reduced itch‑related distress in recent paediatric trials.
What if my pain is linked to nerve damage?
Neuropathic components may need medication like gabapentin. CBT can still assist by lowering anxiety about the pain, but it shouldn't be the sole treatment.
Integrating cognitive-behavioral therapy into your skin‑pain routine can turn a relentless cycle of itch‑pain‑stress into a manageable pattern. Start small, stay consistent, and watch both your mind and skin thank you.


18 Comments
Fabio MaxSeptember 28, 2025 AT 14:05
CBT can really shift the way we experience itch and skin pain; the article does a solid job breaking down the science and practical steps.
Bruce HeintzSeptember 29, 2025 AT 06:45
Totally agree-adding a few minutes of mindfulness each day can make the itch feel a lot more manageable 😊. Keep at it, the gains stack up over weeks.
richard kingSeptember 29, 2025 AT 23:25
The mind‑skin dialogue feels like a secret treaty, where every anxious whisper can summon a flare. If we picture thoughts as tiny messengers, CBT teaches them to rewrite the telegrams that the nervous system receives. By interrogating the “it’s never going to heal” mantra, we strip it of power and let the skin breathe. The article’s step‑by‑step diary suggestion is a brilliant laboratory for personal data. It turns abstract anxiety into concrete numbers you can actually see shifting. When you experiment with not scratching for ten minutes, you witness the brain’s own capacity to dampen sensation. This isn’t magic; it’s a rehearsal of new neural pathways. In the grand theater of chronic itch, CBT hands you the script to rewrite the ending.
Dalton HackettSeptember 30, 2025 AT 16:05
Delving into the evidence, the 2023 UK trial enrolled two hundred adults and delivered eight weekly CBT sessions alongside their usual emollient regimen. Participants reported a striking 38% drop in visual analogue pain scores, a figure that dwarfs the modest 12% reduction seen in the control arm. Such a differential suggests that the cognitive component adds real analgesic value beyond placebo. Moreover, the trial documented improved adherence to moisturiser schedules, hinting that CBT may boost self‑care behaviors. The physiological underpinning lies in stress‑induced cortisol spikes that amplify inflammatory cytokines like IL‑6, a cascade that CBT can blunt through relaxation drills. Neuro‑immune modulation is not merely a hypothesis; functional MRI studies have shown decreased activity in the insular cortex after CBT for chronic itch. Patients also noted a reduction in nighttime awakenings, which translates into better sleep quality and, consequently, faster skin barrier repair. While the study’s sample size was respectable, it nevertheless left open questions about long‑term durability beyond the 12‑week follow‑up. Critics argue that therapist expertise varies, potentially influencing outcomes, yet the standardized manual used mitigates this concern. The authors also performed a subgroup analysis revealing that individuals with higher baseline catastrophizing scores benefited the most, underscoring the relevance of targeting maladaptive thoughts. Interestingly, a parallel 2022 psoriasis trial reported a 45% decline in itch‑related anxiety when CBT was paired with biologic therapy, suggesting synergy across disease phenotypes. These findings collectively bolster the case for integrating psychological training into dermatology clinics. From a practical standpoint, the routine of maintaining a one‑page diary-capturing triggers, thoughts, and pain levels-serves as both assessment tool and therapeutic exercise. The diary’s simplicity makes it accessible even for patients with limited health literacy, provided clinicians give clear instructions. Finally, the cost‑effectiveness angle cannot be ignored; reducing medication reliance and clinic visits through improved self‑management may offset the investment in therapist time.
William LawrenceOctober 1, 2025 AT 08:45
Great, another miracle cure.
Grace ShawOctober 2, 2025 AT 01:25
While the therapeutic promise of CBT is compelling, its implementation must be anchored in rigorous clinical standards. Dermatologists should ensure that any cognitive‑behavioral program is delivered by practitioners with verified credentials in both mental health and dermatologic care. The integration of CBT should complement, not replace, evidence‑based pharmacologic interventions, preserving the central role of moisturisation and anti‑inflammatory agents. Moreover, outcome metrics such as the Dermatology Life Quality Index should be routinely collected to assess real‑world effectiveness. In sum, a multidisciplinary approach maximises patient benefit and safeguards against fragmented care.
Sean PowellOctober 2, 2025 AT 18:05
Totally agree u can mix mind tricks w/ skin meds it works lol
Henry ClayOctober 3, 2025 AT 10:45
CBT? Sure if you have time lol 😒 but not everyone can sit still for weeks
Isha KhullarOctober 4, 2025 AT 03:25
The mind is a battlefield and itch the relentless foe we must outwit
Lila TyasOctober 4, 2025 AT 20:05
Love how the article gives a clear starter routine-especially the 5‑minute breathing drill. It feels doable even on a hectic day, and the diary tip turns vague feelings into concrete data. Keep sharing this kind of practical advice!
Mark SzwarcOctober 5, 2025 AT 12:45
Exactly, the breathing exercise is a low‑cost, high‑impact tool. I’d add that setting a consistent reminder on your phone can help lock the habit in place, reducing the temptation to scratch during stressful moments.
BLAKE LUNDOctober 6, 2025 AT 05:25
It’s fascinating how a simple thought shift can paint a calmer picture on inflamed skin.
Veronica RodriguezOctober 6, 2025 AT 22:05
Absolutely! 😊 Small mental tweaks can ripple into big skin improvements.
Holly HayesOctober 7, 2025 AT 14:45
One must recognise that the naive conflation of psychotherapy with mere pep‑talks belies the nuanced epistemology of cognitive restructuring.
Matthew ShapiroOctober 8, 2025 AT 07:25
Your point about nuance is well‑taken; CBT does rest on a solid evidence base, though it must be delivered with fidelity to the protocol to avoid superficial application.
Julia PhillipsOctober 9, 2025 AT 00:05
Reading about the neuro‑immune bridge felt like watching a secret handshake between brain and skin-so poetic yet scientifically grounded. It gives hope that we can negotiate with our bodies rather than simply endure their rebellion.
Richa PunyaniOctober 9, 2025 AT 16:45
Indeed, the synthesis of neuroscience and psychology presented here offers a compelling roadmap for holistic care. I would encourage clinicians to incorporate brief CBT modules into routine visits, thereby empowering patients with both pharmacologic and cognitive tools.
Bhupendra DarjiOctober 10, 2025 AT 09:25
Good call-blending the two approaches respects both the science and the lived experience of patients, making treatment feel less like a prescription and more like a partnership.