When HIV first became a global crisis, a diagnosis often meant a death sentence. Today, thanks to antiretroviral therapy (ART), people living with HIV can expect to live long, healthy lives - as long as the medications work as intended. But these drugs aren’t simple. They interact with other medicines, your body, and even the virus itself in ways that can undermine treatment. Understanding how these drugs work, why they sometimes fail, and how to avoid dangerous interactions isn’t just for doctors - it’s critical for anyone on treatment.
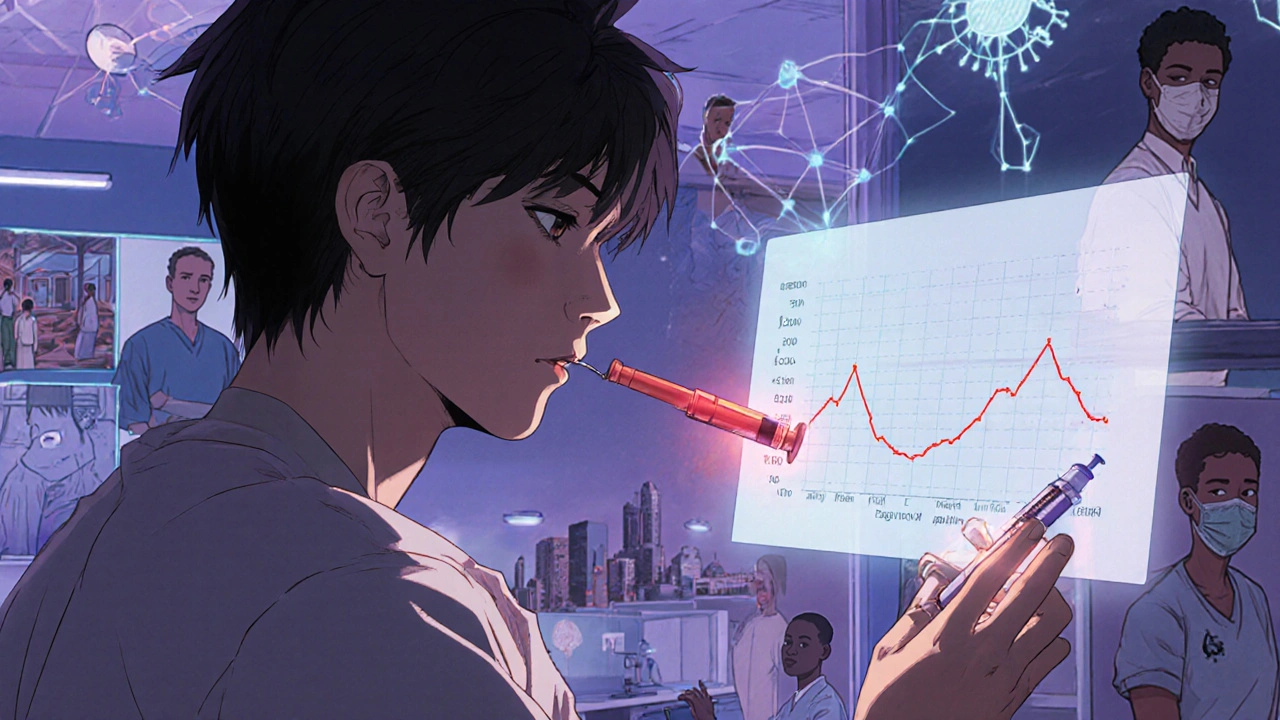
How Antiretroviral Drugs Actually Work
HIV is a sneaky virus. It copies itself inside your immune cells, turning your body into a factory for more virus. Antiretroviral drugs stop this process at different stages. There are six main classes of these drugs, each targeting a different part of the virus’s life cycle.- NRTIs (like tenofovir and lamivudine) trick the virus into using broken building blocks, so it can’t finish copying its DNA.
- NNRTIs (like doravirine and efavirenz) bind to the virus’s reverse transcriptase enzyme and jam it like a wrench in a gear.
- PIs (like darunavir) block the protease enzyme, stopping the virus from maturing into an infectious form.
- INSTIs (like dolutegravir and bictegravir) prevent the virus from inserting its DNA into your cells - the most effective step to block.
- Fusion inhibitors and CCR5 antagonists stop HIV from even entering your cells.
Modern treatment almost always combines at least three drugs from two or more classes. This is called combination ART. Why? Because if one drug fails, the others usually still work. The goal? Reduce the viral load to undetectable levels - below 50 copies per milliliter of blood. When that happens, the virus can’t damage your immune system, and you can’t transmit it to others.
Why Resistance Happens - And Why It’s So Dangerous
HIV mutates quickly. Every time it copies itself, there’s a chance of a mistake. Most of these mistakes kill the virus. But sometimes, a mutation lets it survive despite the drug. That’s resistance.Some drugs are more forgiving than others. INSTIs like dolutegravir and bictegravir are the toughest to resist. It takes multiple mutations for the virus to escape them. NNRTIs like efavirenz? One mutation - K103N - can wipe out their effect. That’s why dolutegravir-based regimens are now the first-line choice in the U.S. and Europe. In clinical trials, only 0.4% of people on dolutegravir developed resistance after two years, compared to 3.2% on efavirenz.
Resistance isn’t just about the drug. It’s about you. Missing doses, even occasionally, creates the perfect environment for resistant strains to grow. A 2025 Reddit survey of over 200 people with HIV found that 68% of treatment failures were linked to missed pills. One user on r/HIV described stopping Atripla because the efavirenz gave him insomnia. Within weeks, his viral load jumped. His virus had developed resistance to both the NNRTI and the NRTI in that combo.
And it’s not just treatment. Even prevention can fail. A case reported in early 2025 involved someone taking Truvada daily for PrEP who still contracted HIV. Testing showed the virus carried the M184V mutation - the same one that makes lamivudine and emtricitabine useless. That means the person was exposed to a strain already resistant to the very drug meant to protect them.
Drug Interactions: When Your Other Medications Fight Your HIV Drugs
Most people with HIV take other medications - for high blood pressure, cholesterol, depression, or even just pain. And many of those can interfere with HIV drugs.Boosted PIs - like darunavir or atazanavir with ritonavir or cobicistat - are especially risky. They slow down how your liver breaks down other drugs. This can cause dangerous buildups. For example:
- Simvastatin (a common statin) is absolutely forbidden with boosted PIs. It can cause muscle damage so severe it leads to kidney failure.
- Midazolam, a sedative used before surgery, can become 8 times more potent, leading to life-threatening breathing problems.
- Some antidepressants, antifungals, and even St. John’s Wort can trigger serious interactions.
Even newer drugs aren’t immune. Doravirine, a newer NNRTI, has far fewer interactions than efavirenz. Only 12% of patients on doravirine needed dose changes for other meds, compared to 35% on efavirenz. That’s why many doctors now prefer doravirine-based combos like DELSTRIGO for patients on multiple medications.
Tenofovir - found in Truvada, Descovy, and Biktarvy - can damage kidneys and bones over time. People switching from tenofovir disoproxil fumarate (TDF) to tenofovir alafenamide (TAF) often see fewer side effects. TAF works at 90% lower doses because it’s better absorbed into immune cells. But it’s still not risk-free. One study found TDF users lost 40% more bone density over three years than those on abacavir.

The Rise of Long-Acting Treatments - And Their Hidden Risks
The biggest shift in HIV care over the last five years? Moving from daily pills to long-acting injections. Cabenuva (cabotegravir + rilpivirine) is given as a monthly shot. The ATLAS trial showed 94% of users preferred it over pills. Fewer pills mean fewer missed doses - and less chance of resistance.But there’s a flip side. If you miss an injection, the drug level in your body drops slowly. That’s different from a missed pill, where the drug vanishes in hours. With injections, subtherapeutic levels can linger for weeks. That’s a breeding ground for resistance. Dr. Sharon Lewin from the University of Melbourne warned at CROI 2025: "Missing one shot doesn’t just mean a gap in protection - it means you’re exposing the virus to just enough drug to teach it how to survive."
Even more advanced options are coming. Lenacapavir, approved in 2022 for multi-drug resistant HIV, is now being recommended by WHO for prevention too - given as a shot every six months. And ViiV Healthcare’s experimental drug VH-184, tested in a small 2025 trial, showed it could knock down even dolutegravir-resistant strains. That’s huge. If it works in larger trials, it could become the new last-resort option.
Testing, Monitoring, and Real-World Challenges
Resistance doesn’t show up overnight. That’s why testing is non-negotiable. Every person newly diagnosed with HIV should get a genotype test - a blood test that scans for known resistance mutations. As of 2025, 82% of newly diagnosed people in the U.S. get this test, up from just 45% in 2015.But access isn’t equal. Rural clinics in the U.S. report 63% difficulty getting test results within 30 days. In sub-Saharan Africa, where 70% of global HIV cases live, only 40% of countries have routine resistance monitoring. That means people there might be on drugs that no longer work - and no one knows.
Doctors use tools like the Stanford HIVdb algorithm to interpret resistance reports. But training varies. Community providers score only 85% accuracy on reading these reports, while infectious disease specialists hit 98%. That gap can lead to wrong treatment choices.
And then there’s cost. Generic tenofovir costs $60 a month. Branded Truvada? $2,800. But doctors rarely switch someone from branded to generic if they’ve had prior treatment - because resistance patterns make it risky. So even when cheaper options exist, they’re not always safe to use.
What You Can Do - Practical Steps for Safer Treatment
If you’re on ART, here’s what actually matters:- Never skip doses. Even one missed pill can create resistance over time. Use pill boxes, alarms, or apps like the Johns Hopkins HIV Guide.
- Tell your doctor everything you take. Supplements, OTC painkillers, herbal remedies - all of it. Don’t assume it’s "not important."
- Ask for resistance testing at diagnosis and after any viral rebound. If your viral load rises, don’t wait. Get tested.
- Know your drug’s side effects. If you’re on TDF and feel bone pain, or on efavirenz and have depression or nightmares, talk to your provider. There are better options.
- Consider long-acting options if you struggle with daily pills. Monthly shots aren’t for everyone, but for many, they’re life-changing.
There’s also good news: with proper care, people on ART now have life expectancies close to the general population. The REPRIEVE trial showed that adding pitavastatin (a statin) to ART cuts heart attack and stroke risk by 36% - especially important for those on PIs, which raise cardiovascular risk by 33%.
The Future: AI, Cures, and Global Equity
Researchers aren’t just fighting resistance - they’re trying to end HIV entirely. The NIH’s Martin Delaney Collaboratories are testing CRISPR gene editing to remove HIV DNA from infected cells. In animal models, they’ve cut viral DNA by 95%. It’s early, but it’s real.AI tools like HIV-TRACE are being integrated into electronic records to predict how resistance spreads between people. That could help public health teams target outbreaks before they grow.
But the biggest challenge isn’t science - it’s access. In the U.S., 57% of people with HIV have suppressed viral loads. In sub-Saharan Africa, it’s 38%. Until we fix that gap, resistance will keep spreading - not because the drugs don’t work, but because not everyone can use them right.
Can I switch my HIV meds if I’m having side effects?
Yes - but not on your own. Side effects like insomnia, bone pain, or mood changes are common reasons to switch. But you need a resistance test first. Switching to a drug your virus is already resistant to can make things worse. Always work with your provider to pick a new regimen based on your virus’s genetic profile.
Is it safe to take supplements with HIV meds?
Some are, many aren’t. St. John’s Wort can drop HIV drug levels by up to 50%, leading to treatment failure. High-dose vitamin C or garlic supplements can interfere with protease inhibitors. Always check with your pharmacist or use the NIH’s HIV Drug Interaction Checker before starting anything new.
Why do some HIV drugs need to be taken with food?
Some drugs, like boosted PIs, need food to be absorbed properly. Taking them on an empty stomach can drop their levels too low, increasing resistance risk. Others, like dolutegravir, work fine with or without food. Always follow the instructions on your prescription - it’s not just a suggestion.
Can I get HIV even if I’m on PrEP?
Yes - but it’s rare. PrEP is 99% effective when taken daily. The cases where it fails usually involve either missed doses or exposure to a drug-resistant strain. That’s why resistance testing is now part of the diagnosis process for anyone who contracts HIV while on PrEP.
What happens if I miss a long-acting injection?
If you miss a monthly injection by more than a week, contact your provider immediately. The drug level drops slowly, so you’re not at immediate risk - but you are at risk for resistance. Your provider may test your viral load and possibly switch you back to pills temporarily. Never skip an injection without talking to your care team.

9 Comments
Andrea GracisOctober 29, 2025 AT 10:59
i just started on Biktarvy last month and honestly? my insomnia is gone but my stomach still feels weird. i didn’t know tenofovir could mess with bones too… i’m gonna ask my doc about TAF next visit.
Matthew Wilson ThorneOctober 31, 2025 AT 01:11
Dolutegravir is the gold standard. Everything else is just noise.
April LiuOctober 31, 2025 AT 22:46
Hey, just wanted to say you’re not alone! 😊 I was on Atripla too-those dreams were *wild*. Switching to Cabenuva changed my life. No more pills, no more panic when I travel. Just one shot a month and I feel like I’m actually living, not just managing. If you’re struggling with side effects, talk to your provider. There’s always a better fit!
Emily GibsonNovember 1, 2025 AT 17:03
It’s wild how much stigma still exists around HIV meds. People act like taking pills every day is some kind of failure. But the truth? Staying on treatment is one of the bravest things you can do. And if you miss a dose? It’s not the end. Just get back on track, test your viral load, and keep going. You’ve got this.
Mirian RamirezNovember 2, 2025 AT 02:39
okay so i read this whole thing and i think i need to write it all down bc i’m terrified i’m gonna forget something. so like, if you’re on ART, never skip pills, even one. i did it once because i was drunk and my viral load spiked. like, 300 copies. not high, but still. my doc said it’s like giving the virus a pep talk. also, st. john’s wort? bad. like, really bad. i took it for anxiety and didn’t know it messed with my meds. big mistake. now i use the NIH drug checker before i even think about taking anything. also, if you’re on TDF and your knees hurt? switch to TAF. my bone density test improved after 6 months. and long-acting shots? i’m on them now and i love it. no more daily panic. but if you miss a shot? call your clinic. don’t wait. the virus doesn’t sleep, and neither should you.
Kika ArmataNovember 3, 2025 AT 14:47
It’s frankly embarrassing that people still think efavirenz is acceptable. The pharmacokinetics are archaic. Doravirine-based regimens have been standard of care since 2021. If your provider is still prescribing Atripla, they’re practicing medicine from 2010. And don’t get me started on the lack of resistance monitoring in sub-Saharan Africa-it’s not a public health issue, it’s a moral failure.
Herbert LuiNovember 5, 2025 AT 09:53
There’s something almost poetic about how HIV forces you to become your own scientist. You learn pharmacology just to survive. You memorize drug names like poetry. You track your viral load like a heartbeat. And in the quiet moments between injections and blood draws, you realize: this isn’t just medicine. It’s a quiet rebellion against time. The virus wants to outlive you. But you? You outlive it. Every pill. Every shot. Every morning you wake up and choose to keep going.
Nick ZararisNovember 5, 2025 AT 19:21
Don’t forget: if you’re on boosted PIs, never take simvastatin-ever. I’ve seen three people end up in the ER with rhabdo. Always check interactions. Always. Use the HIV Drug Interaction Checker. It’s free. It’s reliable. And it could save your kidneys. Also, if you’re on Cabenuva and miss a shot by more than 7 days? Call your clinic immediately. Don’t wait. Don’t hope. Call.
Sara MörtsellNovember 7, 2025 AT 03:25
People act like resistance is a personal failure. It’s not. It’s evolution. The virus isn’t evil-it’s just doing what it’s been doing for 100 million years. We’re the ones who think we can control nature with pills. The truth? We’re playing catch-up. The real solution isn’t better drugs-it’s equity. If someone in rural Uganda can’t get a resistance test, then we haven’t won. We’ve just made the game harder for them. And that’s not science. That’s injustice.