Many older adults take medications every day to manage pain, allergies, bladder issues, or depression. But what if some of those pills are quietly harming their brain? That’s the reality of anticholinergic burden-a hidden risk that’s quietly linked to memory loss, confusion, and even dementia in older adults. It’s not rare. About 1 in 10 seniors in the U.S. are taking at least one drug with strong anticholinergic effects. And most have no idea.
What Exactly Is Anticholinergic Burden?
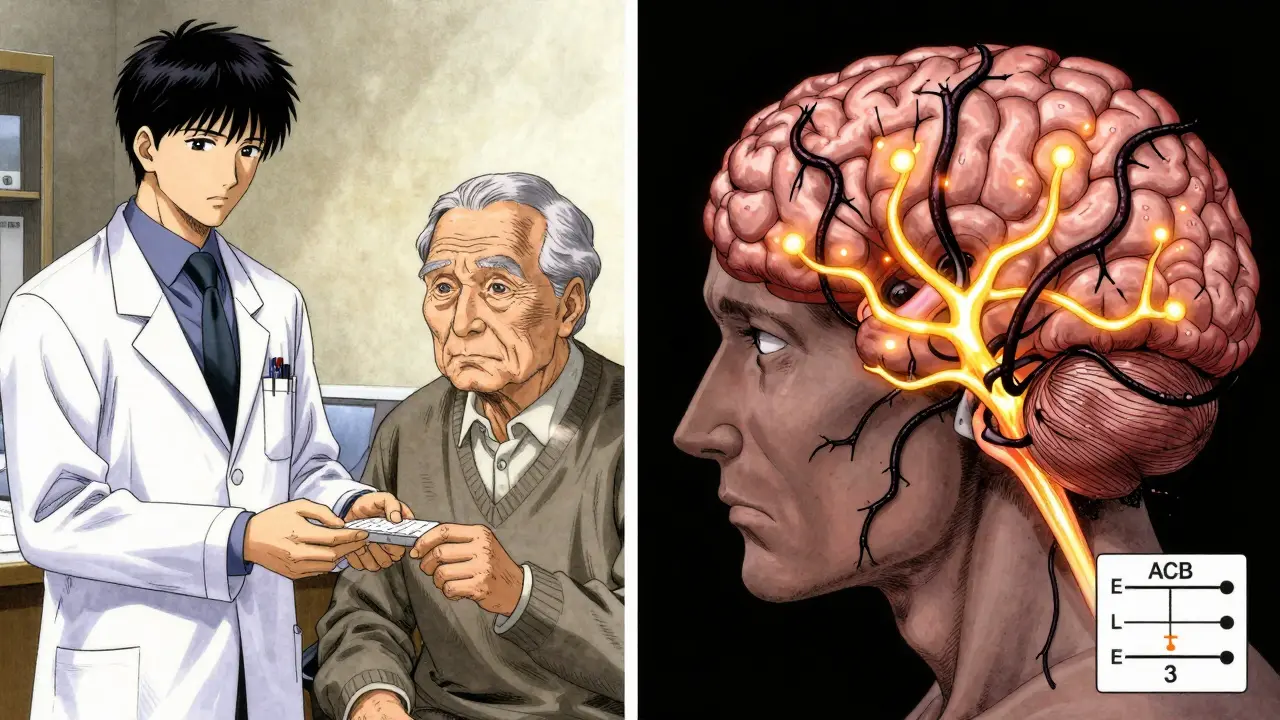
Anticholinergic burden refers to the total effect of all medications that block acetylcholine, a key chemical in the brain that helps with memory, attention, and learning. When this chemical gets blocked, brain signals slow down. It’s like turning down the volume on your brain’s communication system. The more drugs you take with this effect, the louder the silence becomes. There are three main scales doctors use to measure this burden: the Anticholinergic Cognitive Burden (ACB) scale, the Anticholinergic Risk Scale (ARS), and the Drug Burden Index (DBI). The ACB scale is the most widely used today. It rates each medication on a scale from 1 to 3:- Level 1: Mild effect (like some antihistamines)
- Level 2: Moderate effect (like certain bladder medications)
- Level 3: Strong effect (like tricyclic antidepressants or diphenhydramine)
How These Drugs Damage the Brain
Acetylcholine isn’t just about memory-it’s essential for keeping brain cells alive and connected. When anticholinergic drugs block it, especially in the hippocampus and cortex, the brain starts to struggle. Brain imaging studies from JAMA Neurology in 2016 showed that older adults taking even moderate levels of these drugs had 4% less glucose use in areas affected by Alzheimer’s. Glucose is brain fuel. Less fuel means slower thinking. MRI scans from the Indiana Memory and Aging Study found that people on high anticholinergic burden medications lost brain volume faster-0.24% more per year than those not taking them. That’s the equivalent of accelerating brain aging by nearly two years over just three years. These aren’t just imaging quirks. Cognitive tests show real declines. In the ASPREE study of over 19,000 people over 70, each point increase in ACB score meant:- 0.15-point greater yearly drop on word association tests (executive function)
- 0.08-point greater yearly drop on memory recall tests (episodic memory)
Drugs That Carry the Biggest Risk
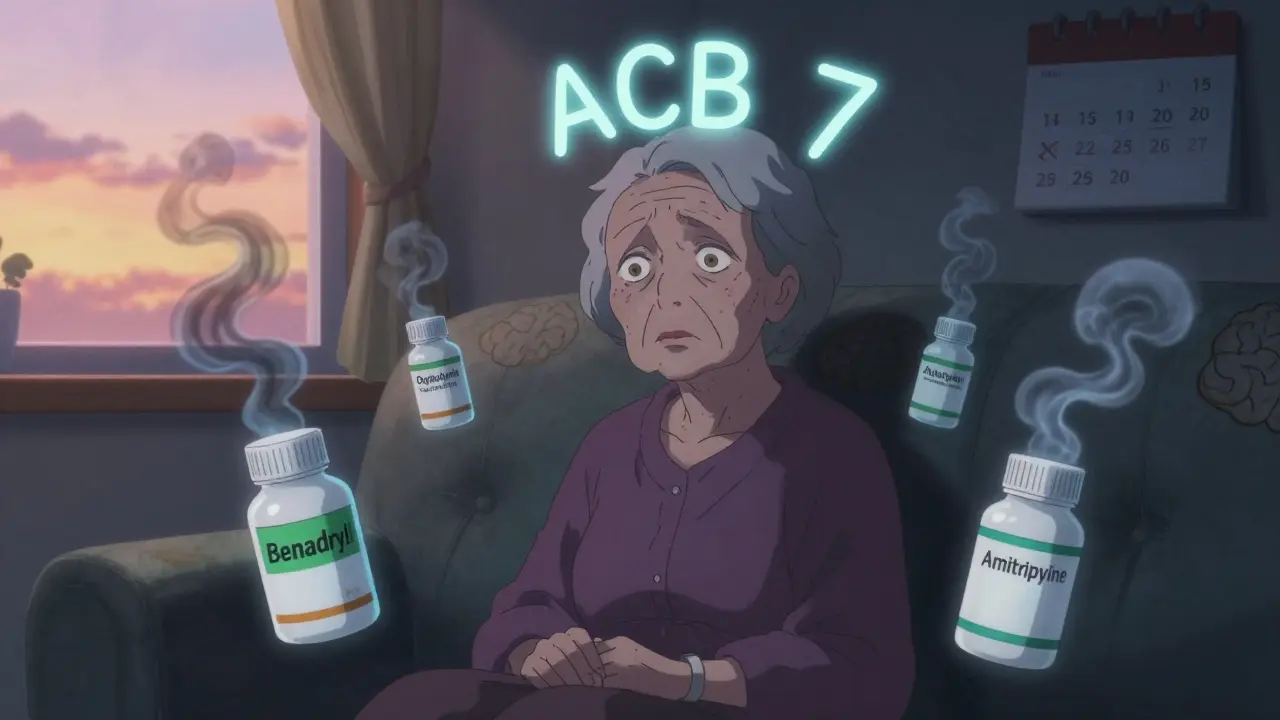
You might be surprised what’s on this list. These aren’t experimental drugs-they’re common, over-the-counter, and often prescribed without warning:- Diphenhydramine (Benadryl, Tylenol PM, Advil PM): Used for allergies or sleep. Level 3. Accounts for nearly 1 in 5 high-burden prescriptions.
- Oxybutynin (Ditropan): For overactive bladder. Level 3. Many seniors take it for years without knowing the brain risks.
- Amitriptyline: A tricyclic antidepressant. Level 3. Still prescribed despite safer options.
- Hydroxyzine: For anxiety or itching. Level 2.
- Chlorpheniramine: Found in many cold and flu meds. Level 2.
Long-Term Use = Higher Dementia Risk
A landmark 2015 study from the University of Washington tracked over 3,400 older adults for more than a decade. Those who took strong anticholinergic drugs for three years or more had a 54% higher risk of developing dementia than those who used them for less than three months. The risk didn’t go up with a single dose-it grew with time. The American Geriatrics Society updated its Beers Criteria in 2023 to explicitly warn against using these drugs in seniors. They’re not just “side effects.” They’re red flags. And the FDA now requires updated warning labels on all anticholinergic medications. Still, many doctors don’t bring it up.Real People, Real Consequences
On AgingCare.com, a caregiver named Jen wrote: “My mom was confused all the time. She’d forget where she was, repeat stories, get lost in her own house. We thought it was early dementia. Then her doctor switched her from oxybutynin to a different bladder med. Within two weeks, she was herself again.” That’s not an isolated story. The FDA’s adverse event database recorded over 1,200 reports of confusion, memory loss, or delirium in seniors linked to anticholinergics between 2018 and 2022. And a 2021 survey found that 63% of seniors were never told about these risks when prescribed these drugs. One woman in her 70s told her pharmacist she’d been taking Benadryl every night for sleep for 15 years. “I didn’t know it could hurt my brain,” she said. “I thought it was harmless.”Can the Damage Be Reversed?
Yes-sometimes. The DICE trial in 2019 followed 286 seniors who slowly stopped their anticholinergic medications. After 12 weeks, their Mini-Mental State Exam (MMSE) scores improved by 0.82 points on average. That’s not a cure, but it’s meaningful. People became more alert, more oriented, more engaged. The catch? It takes time. Withdrawal effects can last 4 to 8 weeks. Some people feel worse before they feel better-dry mouth, constipation, or temporary worsening of the original condition. That’s why stopping these drugs needs to be done slowly, under supervision.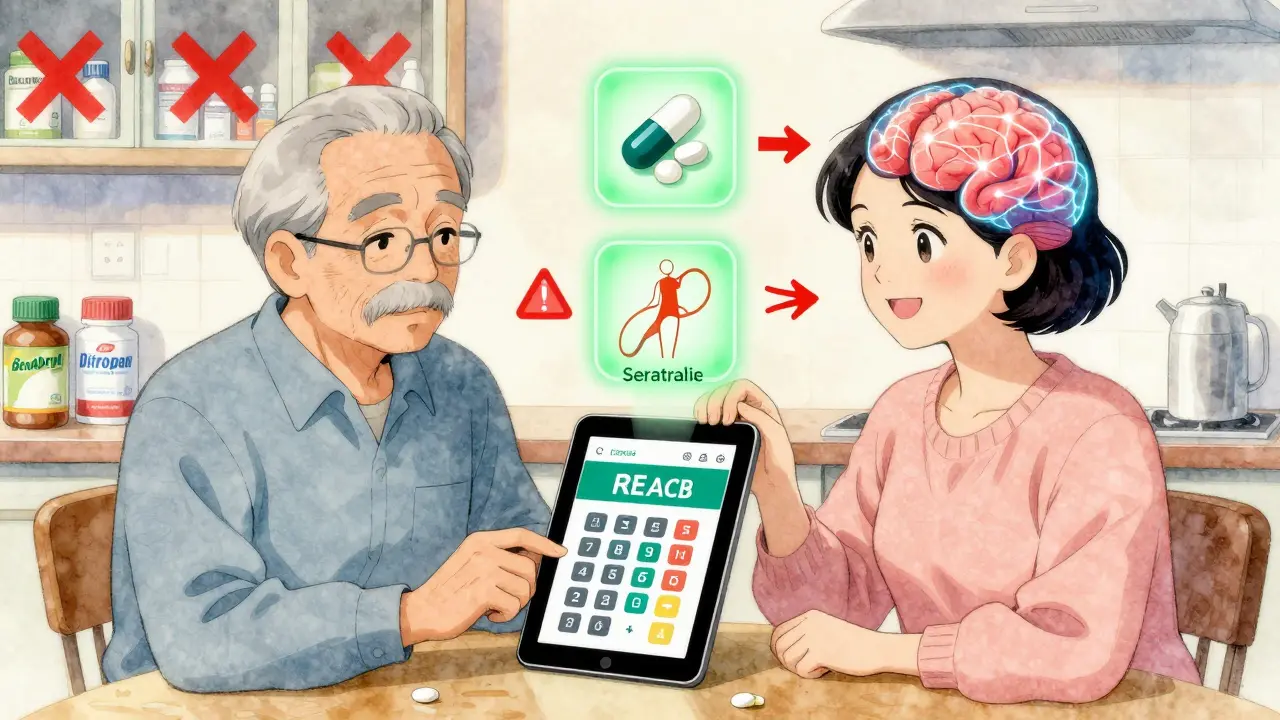
What Can You Do?
If you or a loved one is taking any of these medications, here’s what to do:- Make a full list of every medication-prescription, over-the-counter, and supplements. Include dosages and how often you take them.
- Use the ACB Calculator (launched in 2024 by the American Geriatrics Society). It’s free, available as a mobile app, and instantly scores your burden.
- Ask your doctor: “Is this drug anticholinergic? Is there a safer alternative?”
- Don’t stop cold turkey. Work with your provider to taper off safely.
- Look for alternatives: For sleep, try melatonin or sleep hygiene. For bladder issues, consider pelvic floor therapy or mirabegron. For depression, SSRIs like sertraline have far less brain impact.
Why Is This Still Happening?
The science is clear. The tools exist. So why are so many seniors still on these drugs? One reason: doctors are overwhelmed. A 2021 survey found that primary care physicians need an average of 23 minutes to review a senior’s full medication list. Most appointments are 15 minutes. Another reason: many of these drugs are cheap, familiar, and easy to prescribe. Oxybutynin has been around since the 1980s. Benadryl is on every pharmacy shelf. Pharmaceutical companies are slowly responding. Johnson & Johnson pulled long-acting oxybutynin off the market in 2021. Pfizer pushed solifenacin (VESIcare), which doesn’t cross the blood-brain barrier as easily. But change moves slowly.The Bigger Picture
The Lancet Healthy Longevity Commission now lists anticholinergic burden as one of the top 10 modifiable risk factors for dementia. That means if we eliminated it, we could prevent 10 to 15% of dementia cases in older adults. This isn’t about fear. It’s about awareness. You can’t control aging. But you can control what goes into your body. Medications aren’t harmless. They’re powerful tools-and like any tool, they can hurt if used carelessly. The good news? You don’t need to wait for your doctor to bring it up. You can start today. Look at your medicine cabinet. Ask the questions. Push for safer options. Your brain will thank you.What medications have the highest anticholinergic burden?
The strongest anticholinergic drugs include diphenhydramine (Benadryl), oxybutynin (for bladder control), amitriptyline (an older antidepressant), hydroxyzine, and chlorpheniramine. These are rated Level 3 on the ACB scale and carry the highest risk for cognitive decline. Even over-the-counter sleep aids and cold medicines often contain these ingredients.
Can stopping anticholinergic drugs improve memory?
Yes, in many cases. Studies show that after gradually stopping these medications, seniors often experience improved alertness, clearer thinking, and better memory within weeks. The DICE trial found that after 12 weeks of deprescribing, participants’ cognitive test scores improved by an average of 0.82 points on the MMSE-a meaningful change for daily functioning.
Is it safe to stop taking anticholinergic medications on my own?
No. Stopping abruptly can cause withdrawal symptoms like increased heart rate, worsening of original symptoms (like bladder urgency or depression), or even delirium. Always work with your doctor to create a safe tapering plan. The goal is to replace the medication with a safer alternative, not just remove it.
Are there safer alternatives for common anticholinergic drugs?
Yes. For allergies, use non-sedating antihistamines like loratadine or cetirizine. For overactive bladder, mirabegron is a non-anticholinergic option. For depression, SSRIs like sertraline or escitalopram have minimal brain impact. For sleep, try melatonin, cognitive behavioral therapy for insomnia (CBT-I), or improved sleep hygiene instead of diphenhydramine.
How do I check my anticholinergic burden score?
Use the free ACB Calculator app developed by the American Geriatrics Society in 2024. Simply enter all your medications, and it calculates your total ACB score using the latest scale (version 3.0). A score of 3 or higher is considered high risk. Share the results with your doctor to discuss alternatives.

9 Comments
Anna HungerJanuary 16, 2026 AT 02:29
It's alarming how routinely clinicians prescribe anticholinergics without contextualizing the long-term neurocognitive risks. The ACB scale is not merely a tool-it's a clinical imperative. Patients deserve transparent, evidence-based dialogue about every medication, especially when alternatives exist with negligible central nervous system effects. This isn't speculative medicine; it's a preventable public health crisis rooted in inertia and undereducation.
Susie DeerJanuary 17, 2026 AT 15:57
Stop the fearmongering. Benadryl’s been around since the 1940s and people are still alive. If your grandma’s forgetful maybe she’s just old not poisoned by pills.
TooAfraid ToSayJanuary 18, 2026 AT 16:18
Oh wow so now we’re blaming Big Pharma for seniors being dumb? Maybe the real issue is that people don’t take care of themselves. Sleep on the floor. Drink water. Meditate. Stop popping pills like candy. This whole post is just another way to make people paranoid about medicine so they’ll buy more ‘natural’ nonsense. Also, I heard the FDA is owned by Monsanto. Just saying.
Henry SyJanuary 20, 2026 AT 09:00
Bro I’ve been popping diphenhydramine since I was 22 like it’s gummy vitamins. Now I’m 68 and I still remember my first kiss but can’t recall where I put my damn keys. Is this the brain rot? Or just the natural entropy of being a human who once thought ‘vibes’ were a valid life strategy? Either way, I’m not mad. Just confused. And mildly constipated. Also, my cat judges me. Probably because I smell like a pharmacy.
shiv singhJanuary 21, 2026 AT 01:15
How can you let your parents take these drugs? You’re not a good child if you don’t fight for their brain. I told my aunt to stop all her meds and now she walks barefoot in the garden and chants mantras. Her memory improved. Science is for cowards. Spirituality is the real pharmacology.
Robert WayJanuary 21, 2026 AT 02:04
i was just lookin at my meds and i think i got like 3 of these things?? like benadryl and some bladder thing and i think amitriptyline?? i dont even know what that is but my dr gave it to me for anxiety. oh no oh no oh no. i think i need to go to the er. or maybe just cry in the shower. can someone help me read this chart??
Sarah TriphahnJanuary 22, 2026 AT 07:15
Let’s be real. Most seniors on these meds are just lazy. They don’t want to exercise, they don’t want to sleep better, they don’t want to talk to a therapist. So they take the easy pill. And now they’re surprised their brain is mush? This isn’t a medical failure. It’s a moral failure. Personal responsibility is dead, and we’re all paying for it with dementia bills.
Allison DemingJanuary 22, 2026 AT 22:57
It’s deeply troubling that the medical establishment continues to normalize the prescription of neurotoxic substances under the guise of symptom management. The cumulative impact of even low-dose, long-term anticholinergic exposure is not merely statistical-it is existential. The erosion of acetylcholine signaling represents a quiet, systemic dismantling of cognitive resilience. We are not just treating conditions; we are accelerating neurodegeneration with every unexamined script. This is not a debate. It is a reckoning. And yet, the silence from prescribers remains deafening.
Dylan LivingstonJanuary 24, 2026 AT 10:39
Oh please. You’re telling me that the only reason my 82-year-old aunt can’t remember my name is because she took Benadryl? Not because she’s 82? Not because she watched 12 hours of TikTok a day? Not because she thinks ‘forgetfulness’ is a personality trait? This post reads like a pharmaceutical ad disguised as a public service announcement. Next you’ll tell me sunlight causes wrinkles and oxygen is a silent killer. Meanwhile, my cat is still alive on a diet of tuna and existential dread. Let the elders be.