Anticholinergic Burden Calculator
This tool calculates your total Anticholinergic Cognitive Burden (ACB) score based on all medications you're taking. Higher scores indicate increased risk of cognitive decline and cardiac issues.
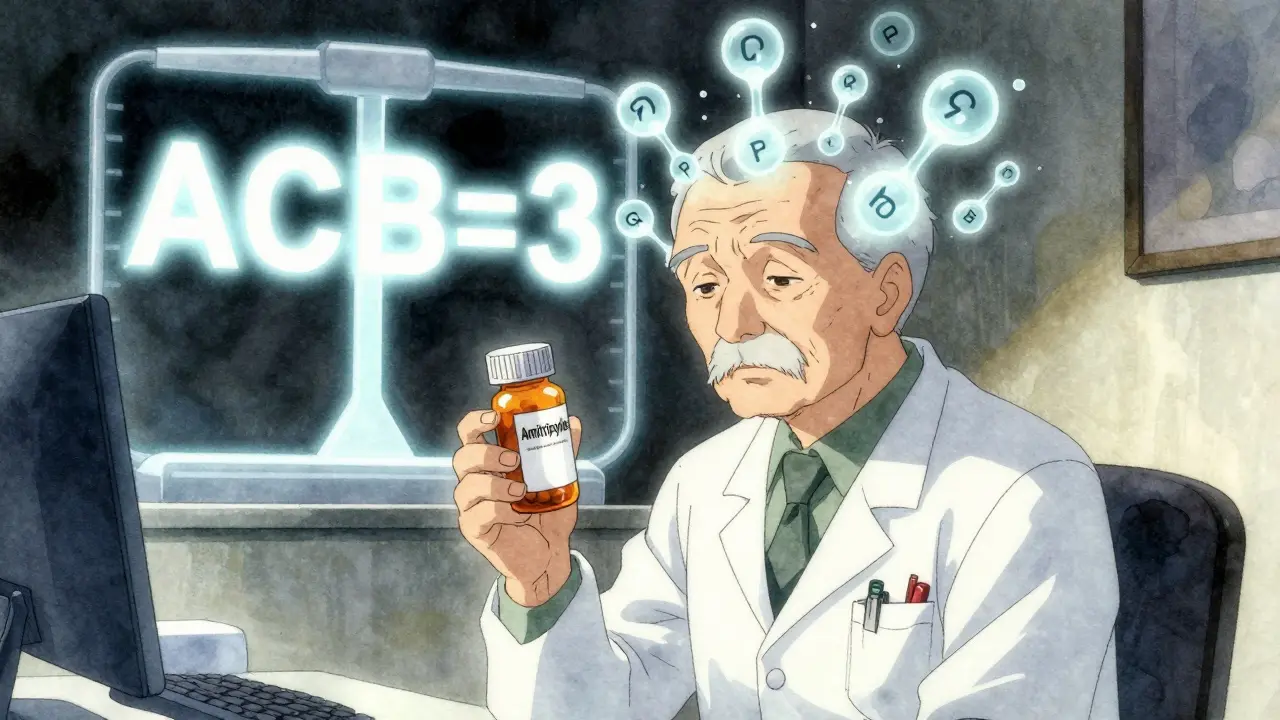
Each medication is assigned an ACB score (1-3) where 3 represents the highest anticholinergic effect. Total score is the sum of all individual scores.
Add Your Medications
Important: Include all prescription drugs, OTC medications, supplements, and even some herbal remedies. Common examples:
- Tricyclic antidepressants: ACB=3 (e.g., Amitriptyline)
- SSRIs: ACB=0-1 (e.g., Sertraline)
- Antihistamines: ACB=1-3 (e.g., Diphenhydramine)
- Bladder medications: ACB=2-3 (e.g., Oxybutynin)
Important Notes: Your ACB score is only one factor in your overall risk. Age, existing health conditions, and other medications also play significant roles. This tool is for informational purposes only and should not replace professional medical advice.
When you’re prescribed a tricyclic antidepressant like amitriptyline or nortriptyline for depression or chronic pain, you’re not just getting a mood stabilizer. You’re also getting a powerful blocker of acetylcholine - a key brain chemical that helps with memory, focus, and even heart rhythm. This is called anticholinergic burden, and it’s not something most patients or even some doctors fully understand until it’s too late.
What Is Anticholinergic Burden?
Anticholinergic burden is the total effect of all the medications in your system that block acetylcholine. Think of it like turning down the volume on your brain’s communication system. Acetylcholine helps neurons talk to each other. When you take drugs that block it, those signals get fuzzy. Tricyclic antidepressants (TCAs) are among the strongest offenders. They were designed to boost serotonin and norepinephrine, but along the way, they also slam shut muscarinic receptors - the same ones targeted by allergy pills, bladder meds, and sleep aids.The Anticholinergic Cognitive Burden (ACB) Scale is the tool doctors use to measure this. It rates drugs from 1 to 3:
- ACB 1 = possible anticholinergic effect
- ACB 2 = definite moderate effect
- ACB 3 = definite strong effect
Every single TCA - amitriptyline, nortriptyline, imipramine - gets an ACB score of 3. That’s the highest possible. Even one pill a day can push your total burden into the danger zone. If you’re also taking diphenhydramine (Benadryl®) for sleep or oxybutynin for bladder issues, your ACB score can quickly hit 5 or 6. And that’s when real risks start piling up.
Cognitive Risks: Mimicking Dementia
One of the most dangerous things about TCAs is how easily their side effects look like dementia. Forgetfulness? Slowed thinking? Trouble finding words? These aren’t just aging. They’re signs your brain is being starved of acetylcholine.A 2022 study tracking over 3,400 adults over 65 for seven years found that people taking medications with an ACB score of 3 or higher had a 54% higher chance of developing dementia. And here’s the kicker - the damage didn’t reverse right away after stopping the drug. Some cognitive decline persisted for years.
Clinicians in the UK and US report cases where older patients were diagnosed with early dementia, only to have their symptoms vanish after switching off amitriptyline. One patient in Birmingham, 72, was told she had mild cognitive impairment. Her family prepared for long-term care. After her GP reviewed her meds and switched her to duloxetine (an SNRI with ACB=0), her memory tests improved within four months. She was able to return to her book club.
That’s not rare. A 2022 survey by the National Council on Aging found 68% of older adults on TCAs had at least two anticholinergic side effects - and 32% said their memory problems were bad enough to consider quitting the drug. The problem? Many don’t connect the dots. They blame aging, stress, or even depression itself.
Cardiac Risks: When Your Heart Can’t Keep Up
It’s not just your brain. Your heart is also at risk.TCAs act like class 1A antiarrhythmics - the same category of drugs used to treat irregular heartbeats. But here’s the twist: they’re not prescribed for that. They’re prescribed for depression. And they can mess up your heart’s electrical system in ways that are hard to predict.
Amitriptyline, in particular, can prolong the QT interval - the time it takes your heart to recharge between beats. A prolonged QT can lead to torsades de pointes, a life-threatening arrhythmia. Studies show amitriptyline carries 2.8 times the risk of QT prolongation compared to sertraline, a common SSRI.
At therapeutic doses, TCAs can slow your heart’s electrical conduction by 10-25%. In overdose, that jumps to 50%. Even at normal doses, patients with existing heart disease - high blood pressure, prior heart attack, or a family history of sudden cardiac death - are at higher risk. One Mended Hearts forum member described how, after three weeks on amitriptyline for depression, he started feeling dizzy and having palpitations. His ER visit revealed a QT interval of 520 milliseconds - well above the safe limit of 450. He was hospitalized and switched to an SSRI within days.
Cardiac toxicity isn’t just theoretical. It’s documented in over 200 case reports in the last decade. And it’s often missed because the symptoms - dizziness, fatigue, skipped beats - get written off as “normal side effects.”
Why Are TCAs Still Prescribed?
If the risks are so clear, why do doctors still use them?Because they work - sometimes better than anything else.
For treatment-resistant depression - when SSRIs and SNRIs have failed - TCAs can be the last resort. They’re also uniquely effective for certain types of chronic pain, especially neuropathic pain from diabetes or shingles. Nortriptyline, in particular, is often used off-label for migraines and fibromyalgia.
But here’s the reality: they’re rarely the first choice anymore. In the U.S., TCA prescriptions for depression dropped from 15% of all antidepressant prescriptions in 2000 to just 4.7% in 2020. In the UK, NICE guidelines since 2018 have explicitly advised clinicians to “minimise the use of medicines associated with increased anticholinergic burden.” The Beers Criteria, used by geriatricians worldwide, lists TCAs as “potentially inappropriate” for adults over 65 - unless no other option works.
Modern alternatives like SSRIs (sertraline, escitalopram) and SNRIs (duloxetine, venlafaxine) have ACB scores of 0 or 1. They’re safer for the brain and heart. Cognitive side effects? Minimal. Cardiac risks? Far lower. That’s why they’ve become the standard.
What Should You Do If You’re on a TCA?
If you’re taking amitriptyline, nortriptyline, or another TCA, here’s what to ask your doctor:- What’s my total ACB score? Include everything - even OTC sleep aids or allergy pills.
- Is this still the best option for me, or have newer, safer drugs become available since I started?
- Could my memory issues or dizziness be linked to this medication?
- Can we try tapering off slowly and switching to something with less anticholinergic burden?
Don’t stop cold turkey. Withdrawal can cause nausea, anxiety, insomnia, and even rebound depression. Tapering over 4-8 weeks is usually safe, especially with nortriptyline, which is slightly less potent than amitriptyline.
Many patients who switch report improvements within months. A 2023 study in Age and Ageing found that older adults who underwent a structured deprescribing program saw their ACB score drop by an average of 4.2 points. Their Mini-Mental State Examination (MMSE) scores - a standard cognitive test - improved by 2.7 points on average. That’s not just a number. It’s the difference between forgetting your keys and remembering them.

The Bigger Picture: A System-Wide Problem
This isn’t just about one class of drugs. It’s about how we prescribe in the age of polypharmacy. Older adults often take five, six, or more medications. Each one adds up. A common combination: amitriptyline for depression, oxybutynin for overactive bladder, chlorphenamine for allergies, and diphenhydramine for sleep. That’s four ACB=3 drugs. Total burden: 12. That’s not just risky - it’s dangerous.Electronic health records in the UK are now starting to flag high anticholinergic burden automatically. NHS Digital piloted an AI tool in 12 trusts that calculates ACB scores in real time when a prescription is written. If a patient is already on a TCA and their GP tries to add a new anticholinergic, the system pops up a warning.
That’s progress. But it’s not enough. Patients need to be educated. GPs need training. And we need to stop accepting “it’s just a side effect” as normal.
Alternatives That Work
You don’t have to stay on a TCA to manage depression or pain. Here are safer, evidence-backed options:- SSRIs (sertraline, escitalopram): ACB=0 or 1. First-line for depression. Low cardiac risk.
- SNRIs (duloxetine, venlafaxine): ACB=0-1. Excellent for depression and neuropathic pain.
- Cognitive Behavioral Therapy (CBT): Proven effective for depression and chronic pain, with no side effects.
- Physical therapies: For pain, options like graded exercise, acupuncture, or nerve blocks can reduce reliance on meds.
- Non-anticholinergic sleep aids: Melatonin, good sleep hygiene, or low-dose mirtazapine (ACB=1) instead of diphenhydramine.
Some patients worry switching will mean losing the benefits. But studies show most people maintain or improve their mood and pain control after switching - without the foggy brain or racing heart.
Final Thoughts
Tricyclic antidepressants have a place - but it’s shrinking fast. Their power comes with a heavy price: memory loss, confusion, and heart rhythm dangers that can be silent until it’s too late. For most people, especially over 50, the risks outweigh the benefits.If you’re on a TCA, don’t panic. But do ask questions. Get your full medication list reviewed. Calculate your ACB score. Explore alternatives. You might be surprised how much clearer your mind feels - and how much steadier your heart becomes - once the anticholinergic fog lifts.

15 Comments
Mussin MachhourDecember 24, 2025 AT 19:23
Man, I switched from amitriptyline to duloxetine last year after my grandma had a scary episode with QT prolongation. Within two weeks, my brain felt like it was no longer wrapped in cotton. No more forgetting where I put my keys. No more dizziness walking up stairs. Honestly? Best decision I ever made. Don’t let doctors push you into old-school meds if there’s a safer way.
Michael DillonDecember 24, 2025 AT 20:34
Everyone’s acting like TCAs are some evil conspiracy. They work. For some of us, SSRIs do nothing. I’ve been on nortriptyline for 12 years. My depression is under control. My heart is fine. Stop fearmongering with ACB scores and let people make their own choices.
Gary HartungDecember 26, 2025 AT 20:11
Let’s be honest-this isn’t about medicine. It’s about the pharmaceutical industry’s quiet war against the elderly. They’ve spent decades pushing SSRIs, SNRIs, and now psychedelics as the ‘new normal.’ Meanwhile, the real solution-lifestyle, therapy, nutrition-is buried under layers of profit-driven guidelines. ACB scores? A distraction. The real issue is that we’ve outsourced our mental health to pills-and now they’re terrified we’ll wake up.
Ben HarrisDecember 27, 2025 AT 15:58
My doctor didn’t even mention the anticholinergic burden when he prescribed me amitriptyline for back pain. I’ve been on it for 5 years. I thought I was just getting older. Turns out I was just getting drugged. I asked for a switch last month. My memory’s already better. My wife says I’ve been more present. Why didn’t anyone tell me this before
Oluwatosin AyodeleDecember 29, 2025 AT 13:50
You Americans are so dramatic. In Nigeria we use amitriptyline for everything-pain, depression, even anxiety. People don’t die from it. They live. Your obsession with side effects is a luxury of the over-medicated West. If you don’t like it, don’t take it. But don’t act like you’re saving lives when you’re just chasing a trend
Justin JamesDecember 29, 2025 AT 20:17
Think about this-what if the ACB scale is just a tool to push you toward more expensive drugs? SSRIs cost 3x more than TCAs. Insurance companies love them. Doctors get paid more to prescribe them. And now suddenly, TCAs are ‘dangerous’? The same drugs that saved millions of people for 60 years? This smells like corporate manipulation. The FDA’s been compromised. The Beers Criteria? Written by consultants with pharma ties. Don’t be fooled. They want you dependent on newer, pricier meds-and they’re rewriting history to make it happen.
Sophie StallkindDecember 31, 2025 AT 11:37
Thank you for this meticulously researched and profoundly important post. The clinical implications of anticholinergic burden, particularly in geriatric populations, are grossly underappreciated in primary care settings. I have personally witnessed multiple cases of iatrogenic cognitive decline attributable to polypharmacy, and I commend the inclusion of evidence-based alternatives. This should be required reading for all medical trainees.
Linda B.January 1, 2026 AT 17:00
Of course the system wants you to stop taking TCAs. Because if you start feeling better without them, you might ask why your depression was ever treated with a drug that makes you forget your own name. And then you might start asking about the real causes. And that? That’s dangerous. Don’t trust the ‘safer alternatives.’ They’re just the next phase of control.
Christopher KingJanuary 1, 2026 AT 21:42
They told me amitriptyline was ‘the last hope’-then I found out my ACB score was 8. My brain felt like a foggy subway station. I switched to sertraline. I cried the first day I remembered my daughter’s birthday. I didn’t even know I’d forgotten it. This isn’t just medicine. It’s a quiet theft of your mind-and no one’s talking about it because they’re too busy selling you the next pill.
Bailey AdkisonJanuary 2, 2026 AT 21:32
Stop using ‘anticholinergic burden’ as a buzzword. The data is real but oversimplified. Many patients benefit from TCAs with no cognitive decline. The real issue is polypharmacy, not TCAs alone. And you didn’t mention that SNRIs carry their own risks-hypertension, withdrawal syndromes, sexual dysfunction. No drug is clean. Stop the moral panic.
Carlos NarvaezJanuary 3, 2026 AT 07:20
TCAs are outdated. Period. If your doctor still prescribes them without a full review, find a new doctor.
Harbans SinghJanuary 4, 2026 AT 02:57
I’m from India and my uncle was on amitriptyline for neuropathic pain for 8 years. He started forgetting names, then his own phone number. We switched him to gabapentin and CBT. He’s back to gardening and telling stories. I wish someone had told us earlier. This info needs to reach people who don’t read medical journals.
Zabihullah SalehJanuary 5, 2026 AT 01:21
It’s funny how we treat the brain like a machine you can tweak with chemicals. We block acetylcholine to fix depression, then wonder why memory fades. Maybe the real problem isn’t the drug-it’s the assumption that we can chemically fix a soul in distress. TCAs don’t heal. They mute. And we call that progress.
Winni VictorJanuary 6, 2026 AT 14:53
So you’re telling me I’ve been taking Benadryl for sleep and amitriptyline for depression and my brain’s been slowly turning into mush? Oh. My. God. I just realized I haven’t remembered what I ate for lunch in three months. I’m switching tomorrow. And I’m telling my whole family. This is a crime.
Jason JasperJanuary 7, 2026 AT 04:37
I’ve been on nortriptyline for 7 years. I’m 68. My mind is sharp. My heart is fine. I’ve had regular EKGs. My ACB score is 3, but I’m not taking anything else anticholinergic. This post is important, but blanket warnings scare people unnecessarily. Medicine isn’t one-size-fits-all. Talk to your doctor. Get tested. Don’t panic. But do ask questions.