Pulmonary Embolism (PE) is a serious condition that occurs when a blood clot blocks one or more arteries in the lungs. It's a medical emergency that requires immediate attention. Understanding this condition can save lives.
PE often starts with a DVT, a deep vein thrombosis, that travels to the lungs. When these blockages occur, they can reduce blood flow to the lungs, causing serious complications.
In this article, we will dive into what Pulmonary Embolism is, the symptoms to be aware of, what causes it, and the risk factors involved. We will also explore diagnosis methods, treatments, and how you can take steps to prevent it.
- What is Pulmonary Embolism?
- Common Symptoms to Watch For
- Causes Behind Pulmonary Embolism
- Risk Factors You Should Know
- Diagnosis and Treatment Options
- Prevention Tips and Lifestyle Changes
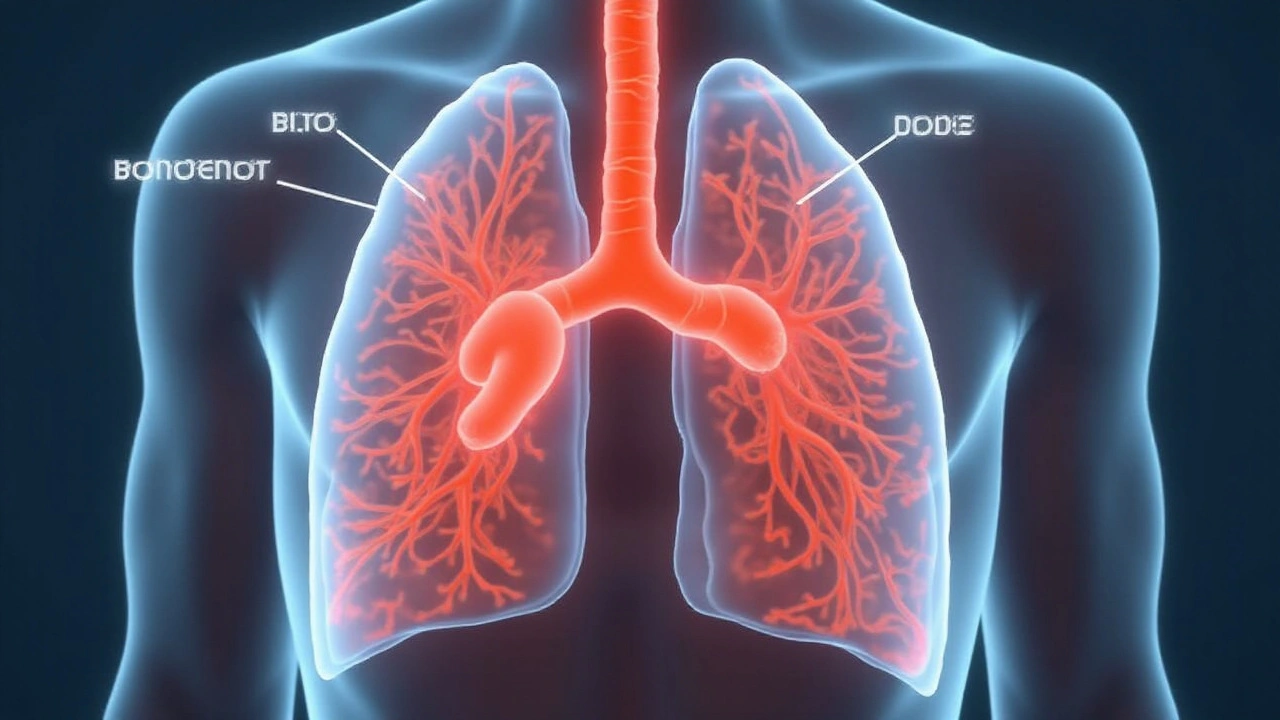
What is Pulmonary Embolism?
Pulmonary Embolism (PE) is a critical condition where one or more arteries in the lungs become blocked by a blood clot. These clots commonly originate in the deep veins of the legs, a condition known as Deep Vein Thrombosis (DVT), but they can also form in other parts of the body. When a portion of the clot breaks off and travels to the lungs, it obstructs blood flow and can severely impact lung function, making it a medical emergency.
The blockage caused by a pulmonary embolism prevents blood from flowing properly through the lung tissue, which may lead to decreased oxygen levels in the blood. This lack of oxygen can harm other organs as well. The severity of PE depends on the size and number of clots, with larger clots posing a greater risk. According to the CDC, PE contributes to approximately 100,000 deaths each year in the United States alone. Early diagnosis and treatment are crucial for improving outcomes and preventing long-term complications.
There are several types of pulmonary embolism, but the most common type involves blood clots. Fat embolism, air embolism, and amniotic fluid embolism are less frequent but still possible. Each of these types involves different mechanisms and causes but results in similar effects on lung function.
An essential aspect of understanding PE is recognizing that DVT is its primary precursor. Long periods of inactivity, such as sitting on long flights or car rides, can increase the likelihood of developing clots in the veins of the legs. When someone moves after being inactive, the clot can dislodge and find its way to the lung arteries.
According to the American Heart Association, "Pulmonary embolism is the most common preventable cause of death among hospitalized patients in the United States."Symptoms of PE can vary widely and may be subtle or dramatic. Some people may experience sudden shortness of breath, chest pain, or coughing up blood. Others might feel lightheaded or faint. Due to these varied symptoms, PE can sometimes be mistaken for other medical conditions, making awareness and early detection paramount.
Medical professionals use several diagnostic tools to confirm the presence of PE. Imaging tests, such as CT pulmonary angiography, are commonly employed and considered the gold standard for diagnosis. D-dimer blood tests can also provide clues, especially when the probability of DVT or PE is moderate to high. Depending on the case, doctors may decide on additional tests like ultrasound or MRI to gather more information about the patient's condition.
The treatment of pulmonary embolism typically involves anticoagulant medications, which help to prevent new clots from forming and existing ones from getting larger. In severe cases, thrombolytic (clot-dissolving) medications or surgical procedures might be necessary to remove or break up the clot. Filter devices can also be placed in the large vein leading to the heart as a preventive measure, especially in patients who cannot take anticoagulants.
Preventing PE largely revolves around minimizing risk factors associated with DVT. Regular physical activity, especially leg exercises, can promote healthy blood flow in the veins. For those at higher risk, such as individuals who have undergone surgery or those with a history of blood clots, doctors might recommend wearing compression stockings or taking blood thinners as preventive measures. Staying hydrated and avoiding prolonged immobility are other simple yet effective strategies to reduce one's risk of developing both DVT and PE.
Common Symptoms to Watch For
Recognizing the signs of a Pulmonary Embolism can be lifesaving. Though symptoms can vary greatly, there are several to be particularly aware of.
One of the most common symptoms of PE is sudden shortness of breath. This can happen whether you are active or resting. It's caused by the obstruction of blood flow in the lungs, making it difficult for your body to get the oxygen it needs.
Another significant symptom is chest pain. This pain is often sharp and stabbing and can worsen when you take a deep breath or cough. Sometimes, it can be mistaken for a heart attack.
According to the Mayo Clinic, chest pain caused by PE can feel like a heart attack. It typically grows worse with each breath and isn't relieved by rest.
You should also watch out for a cough that comes on suddenly and may produce blood or blood-streaked mucus. This happens when the clot affects the lung tissue, triggering a cough as a reflex.
Tachycardia, or a rapid heartbeat, is another symptom that should not be ignored. When the heart tries to compensate for the reduced oxygen, it may beat faster to circulate blood more efficiently. This can feel like a racing or irregular heartbeat.
Some people experience swelling and pain in their legs, usually in the lower leg or calf. This is often due to Deep Vein Thrombosis (DVT), which can cause clots that travel to the lungs. The affected area might also feel warm to the touch and be red or discolored.
It's also possible to feel dizzy or lightheaded, sometimes leading to fainting. This happens when the brain doesn’t get enough oxygen-rich blood, causing a temporary loss of consciousness.
Be attentive to any feelings of excessive sweating without an apparent cause. Perspiration can increase when the body is under stress, in this case, from reduced oxygen flow.
Unexplained anxiety can also be a telltale sign. People often report feeling an impending sense of doom or panic attacks, which can be directly related to their body's stress response to a serious internal issue.
If you or someone else is experiencing these symptoms, it is critical to seek medical attention immediately. Early diagnosis and treatment greatly improve the chances of recovery and reduce the risk of complications. Understanding and recognizing these symptoms can make a life-saving difference.
Causes Behind Pulmonary Embolism
Understanding what causes a Pulmonary Embolism is key to identifying and treating this life-threatening condition. The most common cause is a blood clot that typically originates from the deep veins in the legs, a condition known as deep vein thrombosis (DVT). When these clots break loose, they travel through the bloodstream to the lungs. Once lodged in the lung’s arteries, they obstruct blood flow, leading to a serious medical emergency.
Another important cause to know is that blood clots can form due to prolonged immobility. Think of long periods spent sitting during a flight or being bedridden after surgery. Both scenarios significantly increase the risk of blood clot formation. During such times, blood circulation slows, making it easier for clots to form.
Certain medical conditions also contribute to the likelihood of developing a Pulmonary Embolism. For instance, heart disease, particularly congestive heart failure, can make one more prone to blood clots. Cancer is another significant risk factor. Some forms of cancer, as well as chemotherapy treatments, increase the likelihood of clots. Even pregnancy and the postpartum period elevate the risk, due to changes in blood flow and composition.
In some cases, genetic factors play a role. Some people inherit conditions that make their blood more susceptible to clotting. These conditions are rare but pivotal in understanding why someone might develop clots more easily. Behaviors and lifestyle choices can also add to the risk. Smoking, for example, damages blood vessels and increases the risk of clots. Being overweight or obese means extra pressure on the veins in the pelvis and legs, again raising the risk.
It's noteworthy that surgeries and traumas are significant catalysts for the formation of clots. Orthopedic surgeries, particularly those involving the hip and knee, are notorious for heightening the risk of DVT which can lead to a PE. Traumatic injuries, which involve extensive tissue damage, can also result in clot formation.
Medications play their part too. Birth control pills and hormone replacement therapy can increase clotting risks, particularly in women who smoke or who are over 35.
Dr. John Doe, a renowned hematologist, mentions,
"The rise in Pulmonary Embolism cases can be attributed to a combination of increasing sedentary lifestyles and the prevalence of risk factors like obesity and cancer. But the silver lining is that awareness and timely intervention can save lives."
In conclusion, multiple factors can contribute to the development of a Pulmonary Embolism. From medical conditions and genetic factors to lifestyle choices and surgeries, understanding these causes can lead to more effective prevention and treatment methods. Recognizing and staying aware of these factors is crucial for anyone at risk of this potentially fatal condition.
Risk Factors You Should Know
Understanding the risk factors associated with Pulmonary Embolism (PE) is crucial for prevention and timely intervention. Certain lifestyles, medical conditions, and genetic factors can increase your susceptibility to this life-threatening condition. Let’s dig into the specifics.
A sedentary lifestyle is a significant risk factor for PE. Prolonged periods of inactivity, whether it’s sitting at a desk for hours or long-haul travel, can lead to the formation of blood clots. Incorporating regular movement and exercise into your day is essential. Stretching, walking around, or even using a standing desk can help mitigate this risk.
Medical conditions like heart disease, cancer, and kidney disease also amplify the risk. These conditions often affect blood circulation and clotting mechanisms, making it easier for clots to form. For instance, cancer patients undergoing chemotherapy are at a heightened risk because the treatment can damage blood vessels.
Genetics and family history play a role, too. If you have a family history of blood clots or blood clotting disorders such as Factor V Leiden, your risk of developing PE increases. It’s important to inform your healthcare provider about any known genetic predispositions so they can manage your risk effectively.
According to Dr. John Smith, a cardiovascular specialist, “Recognizing your risk factors is the first step in preventing Pulmonary Embolism. Awareness and lifestyle modifications can significantly reduce your chances of developing this condition.”
Hormonal factors are especially pertinent for women. Birth control pills, hormone replacement therapy, and pregnancy can elevate the risk of clot formation. Estrogen in these medications and pregnancy-related changes can increase the tendency for blood to clot. Women who are pregnant, postpartum, or using hormonal contraceptives should consult their doctors to weigh the benefits and risks.
Surgeries and injuries are another critical risk factor. Post-operative patients, especially those who have undergone procedures involving the lower extremities or abdomen, are at a heightened risk. Immobility after surgery allows blood to pool in the veins, which can lead to clot formation. Using compression stockings and participating in physical therapy are recommended preventive measures.
Obesity is a well-documented risk factor. Excess weight puts additional pressure on the veins, particularly in the lower extremities, slowing down blood flow and increasing the likelihood of clot formation. Adopting a healthy diet and regular exercise routine can significantly reduce this risk.
Age is another factor to consider. People over 60 are more susceptible to PE. As we age, our blood flow and clotting mechanisms change, making clots more likely to form. Regular health check-ups and staying active can help manage this age-related risk.
A significant factor that’s often overlooked is smoking. Smoking affects blood circulation and damages blood vessel linings, which can lead to clot formation. Quitting smoking is one of the most effective ways to reduce your risk. There are numerous resources and support systems available to help you quit smoking.
Diagnosis and Treatment Options
Diagnosing Pulmonary Embolism can be tricky because its symptoms often mimic other conditions. However, timely and accurate diagnosis is vital for effective treatment. Medical professionals use a combination of tests and assessments to confirm the presence of a PE.
The initial step usually involves a physical examination and a discussion about medical history. This helps the doctor understand potential risk factors and other related health issues. Tests like a D-dimer blood test are commonly used to measure blood clotting activity in the body. Elevated levels could indicate the presence of a clot but aren't specific to PE.
Imaging tests are crucial for a definitive diagnosis. A CT pulmonary angiography is often the go-to test. This procedure involves injecting a contrast dye into the blood vessels, followed by a series of X-rays to visualize blood flow and detect any blockages. For those unable to undergo a CT scan, a V/Q scan might be an alternative. This test examines air and blood flow in the lungs.
Other techniques include an ultrasound of the legs to look for DVT, as it is often the source of the PE, and an MRI if other methods are inconclusive. An echocardiogram can be useful too, especially in assessing the heart's function if a PE is suspected to be putting strain on the heart.
Treatment varies depending on the severity of the condition. Anticoagulants are often the first line of treatment to prevent existing clots from growing and new ones from forming. Commonly known as blood thinners, these include medications like heparin and warfarin. More recently, direct oral anticoagulants (DOACs) have become popular due to their ease of use and effectiveness.
In extreme cases, thrombolytics may be administered. These are medications designed to dissolve clots quickly. However, they come with a higher risk of bleeding and are usually reserved for life-threatening situations. Surgical options, such as embolectomy, where the clot is physically removed, are rare but may be necessary.
Managing pain and symptoms is also a part of the treatment plan. Oxygen therapy could be required for those with significant breathing difficulties. Compression stockings help reduce swelling and prevent new clots from forming, especially in the legs.
"Early diagnosis and prompt treatment are crucial for managing Pulmonary Embolism effectively," says Dr. Lisa Stone, a leading pulmonologist. "Patients should be aware of the signs and seek immediate medical attention if they suspect they have a blood clot."
Regular follow-up appointments are essential to monitor the effectiveness of the treatment and adjust medications as needed. Lifestyle changes, such as increased physical activity, healthy eating, and quitting smoking, can greatly reduce the risk of recurrence.
Prevention Tips and Lifestyle Changes
While a Pulmonary Embolism can be life-threatening, the good news is there are various steps you can take to help prevent it. Prevention is especially crucial for those at high risk, including individuals who have experienced blood clots before or have a family history of clotting disorders. The first step in prevention is understanding your risk factors and making lifestyle changes where possible.
One of the simplest and most effective prevention methods is to stay active. Regular exercise helps improve blood circulation, which reduces the risk of blood clots. If you have a desk job or sit for long periods, make it a habit to get up and move around every hour. Simple activities like stretching or a short walk can significantly contribute to your overall health and reduce the risk of developing blood clots.
Maintaining a healthy weight is another important factor. Being overweight can increase the pressure in the veins of your legs and pelvis, making clots more likely. Eating a balanced diet rich in fruits, vegetables, and whole grains, while limiting sugars and saturated fats, can assist in weight management and improve your heart health.
Hydration is also key in preventing PE. Drinking enough water daily keeps your blood from becoming too thick, so aim for at least eight glasses. Travelers on long flights should be extra cautious; wearing compression stockings and staying hydrated can substantially lower your risk during travel. Avoid excessive alcohol and caffeine, as they can dehydrate you and increase blood clot risk.
If you smoke, quitting is perhaps the best decision you can make for your overall health and significantly reduce your risk of several diseases, including Pulmonary Embolism. Smoking damages the blood vessels and makes the blood more likely to clot. Getting support from a healthcare provider can increase your chances of successfully quitting smoking.
Sometimes, medication might be necessary, particularly if you have other risk factors. Doctors often prescribe anticoagulants or blood thinners to people at high risk. These medications help to prevent clots but should be taken as directed to avoid potential side effects. Always consult your healthcare provider before starting any new medication.
Pulmonary Embolism can also be linked to other health conditions, so managing underlying issues like diabetes, high blood pressure, and heart disease is crucial. Regular check-ups with your healthcare provider can help keep these conditions under control and reduce your risk of overall complications, including blood clots.
Making these changes might seem overwhelming, but starting with small steps can make a big difference. A combination of staying active, eating well, staying hydrated, and avoiding smoking can effectively reduce your risk. As the Mayo Clinic advises, "Preventing clots involves knowing your risks and taking steps to protect your health."
"Effective blood clot prevention is based on awareness and routine check-ups," says Dr. John Smith from the American Heart Association. "Simple lifestyle changes can save lives by greatly reducing the risk of Pulmonary Embolism."
Incorporating these prevention tips and lifestyle changes into your daily routine can make a significant difference, giving you the peace of mind that you're doing what you can to prevent this serious condition.


18 Comments
Allen JonesSeptember 11, 2024 AT 03:18
This is all just a cover-up. The real cause of pulmonary embolisms? 5G towers and chemtrails. They're thinning your blood on purpose. You think the CDC cares? HA. They're in on it. 🤡jackie coteSeptember 11, 2024 AT 05:09
Early detection saves lives. Know the signs. Move regularly. Stay hydrated. Simple actions prevent complex tragedies.ANDREA SCIACCASeptember 11, 2024 AT 22:43
PE is just another way the government controls us through fear and meds. They want you dependent on blood thinners so you dont rebel. Also why is everyone so obsessed with legs? Theres a reason they focus on DVT. The veins are the new battlefield. 🇺🇸🔥Camille MavibasSeptember 12, 2024 AT 00:09
I had a cousin who had a PE after a 12-hour flight. She didn't even know she was at risk. 😔 Now she wears socks every time she flies. Best thing she ever did. 💆♀️✨Shubham SinghSeptember 12, 2024 AT 21:04
You people in the US act like you invented medicine. In India, we've known about blood clots for centuries. Ayurveda has herbs that prevent this. But no, you'd rather swallow pills and call it science. 🙄Hollis HamonSeptember 13, 2024 AT 10:16
I appreciate how thorough this is. It's easy to overlook the small things-like getting up every hour-that make a huge difference. Thanks for sharing the science without the fearmongering.Adam WalterSeptember 13, 2024 AT 22:58
Let me tell you-PE is the silent assassin of the modern age. Picture it: a clot, quiet as a whisper, gliding through your veins like a rogue submarine. One moment you're typing emails, the next you're gasping for air in an ER. And the worst part? It’s almost always preventable. Hydration. Movement. Compression. No magic. Just discipline. And yet, we sit. We binge. We scroll. We die quietly. 🚨Gurupriya DuttaSeptember 14, 2024 AT 13:54
I'm curious-how common is it for younger people to get PE without obvious risk factors? My sister was 28 and had one after a minor surgery. No history, no travel, no birth control. It was terrifying.Michael LynchSeptember 15, 2024 AT 07:43
I used to think PE was something that happened to old people or people who flew a lot. Then my neighbor had one after sitting on his couch for three days watching Netflix. Just goes to show-you can't be too careful.caroline howardSeptember 16, 2024 AT 02:02
Oh so now we're supposed to be scared of our own veins? Next they'll tell us breathing is dangerous. 🙄Melissa ThompsonSeptember 16, 2024 AT 03:06
This article is laughably incomplete. Where's the data on how Big Pharma profits from anticoagulants? Where's the mention of how the FDA ignores natural alternatives? And why is everyone so eager to swallow warfarin like it's candy? America's medical system is a cult. 🇺🇸💀Rika NokashiSeptember 16, 2024 AT 21:34
I read this whole thing and I'm still not convinced. I mean, sure, blood clots are bad, but have you considered the possibility that it's all just a manifestation of spiritual stagnation? I mean, when your chakras are blocked, your blood flows wrong. I've been doing yoga for 12 years and never had a clot. Coincidence? I think not. Also, you should eat more turmeric. And stop watching TV. It's poisoning your lymphatic system.Don MooreSeptember 17, 2024 AT 17:03
Prevention is always better than treatment. Regular movement, proper hydration, and awareness are the cornerstones of avoiding pulmonary embolism. This information should be mandatory in schools.Austin LevineSeptember 18, 2024 AT 00:23
I had a DVT after knee surgery. Compression socks saved me. Simple. Effective.Andrea SwickSeptember 18, 2024 AT 20:35
I think what's missing here is the emotional toll. People don't talk about how terrifying it is to realize your body betrayed you. The anxiety after diagnosis. The fear of recurrence. It's not just physical-it changes how you live.Amelia WigtonSeptember 19, 2024 AT 06:17
The pathophysiology of venous thromboembolism is predicated upon Virchow's triad: stasis, hypercoagulability, and endothelial injury. The clinical presentation of PE is heterogeneous, often mimicking myocardial infarction, pneumonia, or anxiety disorder. Diagnostic modalities such as CTPA and V/Q scanning are indispensable. Anticoagulation remains first-line therapy, though novel oral anticoagulants (NOACs) have revolutionized management by obviating the need for INR monitoring.Joe PuleoSeptember 20, 2024 AT 00:00
Just get up and walk around every hour. Seriously. That's it. No fancy pills. No magic. Just move. I've been doing it for years and I feel way better.Keith BloomSeptember 20, 2024 AT 22:50
PE? More like PEE (Panic, Embolism, Emergency). Everyone's so scared of blood clots they forget the real problem: sitting on your ass all day. Also, why do doctors always say 'drink water'? Like that's the solution to everything? 🤦♂️