When your lower back aches after standing too long, and your hamstrings feel like they’re tied in knots, it’s easy to blame bad posture or a tough workout. But if the pain sticks around for weeks, radiates down your legs, or makes walking feel like a chore, you might be dealing with something deeper: spondylolisthesis. It’s not just a slipped disc-it’s a vertebra that’s actually slid forward out of place, pressing on nerves and throwing your spine out of alignment. Around 6% of adults have it, and many don’t even know until the pain forces them to see a doctor.
What Exactly Is Spondylolisthesis?
Spondylolisthesis comes from Greek words meaning "vertebra" and "slip." It happens when one of the bones in your lower spine-most often the fifth lumbar vertebra (L5)-slides forward over the one below it, usually the sacrum (S1). This isn’t a sudden injury for most people. It’s a slow creep, often caused by years of wear and tear, genetics, or repetitive stress from sports like gymnastics or football. There are five main types:- Degenerative-the most common in adults over 50. Arthritis breaks down the joints and discs, letting the vertebra slip.
- Isthmic-caused by a tiny fracture in the pars interarticularis, a thin bone bridge connecting spinal joints. Often starts in teens or young adults who do a lot of backward bending.
- Dysplastic-a birth defect where the spine never formed right.
- Pathologic-due to diseases like bone cancer or osteoporosis weakening the bone.
- Traumatic-from a direct injury, like a car crash or fall.
Doctors grade the slip using the Meyerding scale, from Grade I (less than 25% slippage) to Grade IV (over 75%). Most people have Grade I or II. Only about 1 in 4 have a high-grade slip, but those are the ones more likely to need surgery.
Why Does It Hurt? The Real Symptoms
Not everyone with spondylolisthesis feels pain. In fact, up to half of people have no symptoms at all. But if you do, here’s what you’re likely to feel:- Lower back pain that feels like a deep muscle strain, worse when standing or walking, better when sitting or leaning forward.
- Pain or tingling that shoots into your buttocks, thighs, or even calves-like sciatica.
- Tight hamstrings. Seriously. About 70% of people with this condition can’t touch their toes without discomfort.
- Stiffness in the lower back, especially in the morning.
- Difficulty walking long distances. Some people have to stop and lean on a cart or wall because their legs go numb or weak.
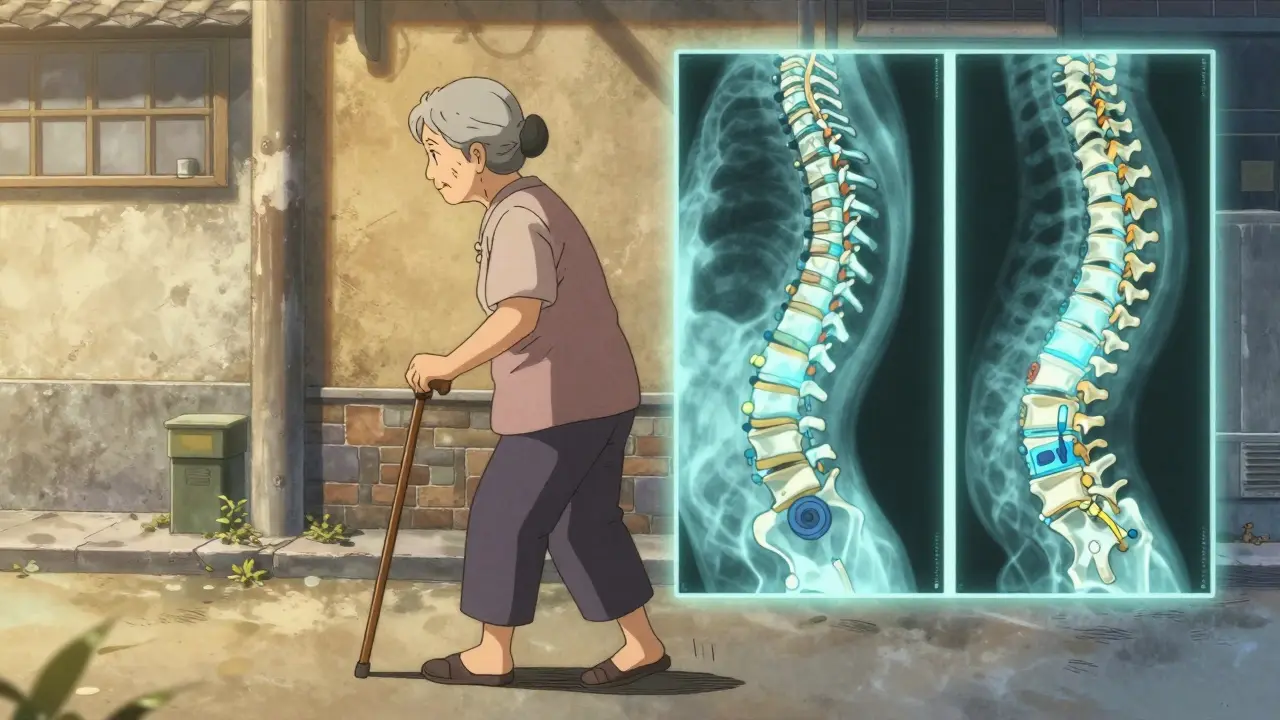
If the slip is severe (Grade III or IV), you might also notice a visible change in your posture-your back looks more curved than usual, or you develop a rounded upper back as your spine tries to compensate. That’s called kyphosis. It doesn’t happen overnight, but over time, your body’s trying to keep you balanced.
How Do You Know for Sure?
A doctor won’t guess. They’ll want images. The first test is usually a standing lateral X-ray. That’s key because the slip can look worse when you’re upright than when you’re lying down. If the X-ray shows a slip, they’ll likely order an MRI to see if any nerves are being squished. A CT scan might follow to get a clear picture of the bone structure-especially if they’re thinking about surgery.Don’t be surprised if your doctor asks about your activity level. Athletes under 25 with sudden back pain? They’ll check for isthmic spondylolisthesis. Someone over 60 with chronic low back pain? Degenerative is the likely culprit. Age and lifestyle matter as much as the X-ray.
Conservative Treatment: What Works (and What Doesn’t)
Most people don’t need surgery. In fact, 80% of cases improve with non-surgical care. The goal isn’t to pull the bone back into place-it’s to reduce pain, strengthen your core, and take pressure off your spine.- Physical therapy is the cornerstone. A good program focuses on core stability (transverse abdominis and multifidus muscles), hamstring stretches, and posture training. Most people see real improvement after 12 to 16 weeks of consistent sessions. But here’s the catch: only about 65% stick with it long enough.
- NSAIDs like ibuprofen or naproxen help with inflammation and pain. But they’re not a long-term fix. If you’re using them daily for months, talk to your doctor about stomach or kidney risks.
- Epidural steroid injections can give temporary relief if nerve pain is sharp and shooting. They don’t fix the slip, but they can buy you time to heal with PT.
- Activity modification means avoiding things that make it worse-like heavy lifting, backbends, or high-impact sports. If you’re a runner or a gymnast, you’ll need to switch to swimming or cycling for a while.
And yes, if you smoke, quitting isn’t just good advice-it’s critical. Smokers have more than three times the risk of failed fusion if surgery becomes necessary. If you’re overweight, losing even 5-10% of your body weight can cut your pain significantly.
Fusion Surgery: The Big Decision
Surgery isn’t for everyone. But if you’ve tried 6 to 12 months of conservative care and you’re still in pain, can’t walk more than a block, or your legs are going numb regularly, it’s time to talk about fusion.Spinal fusion means joining two vertebrae together so they heal into one solid bone. It stops the slip from getting worse and takes pressure off the nerves. There are three main types:
- Posterolateral fusion-the traditional method. Bone graft is placed along the back of the spine, and screws and rods hold everything in place. Works well for Grade I-II slips (75-85% success), but less reliable for higher grades.
- Interbody fusion (PLIF/TLIF)-the surgeon removes the damaged disc and inserts a spacer filled with bone graft between the vertebrae. This restores disc height and opens up the space where nerves exit. Success rates are higher-85-92% across all grades. This is now the go-to for most surgeons.
- Minimally invasive fusion-smaller incisions, less muscle damage, faster recovery. Used in about 10% of cases. Not always an option if the slip is severe or there’s major instability.
Recent advances include new FDA-approved interbody devices that help correct the slip better during surgery. And in 2023, a trial showed that adding bone morphogenetic protein (BMP-2) to the graft boosted fusion rates to 94% in high-risk patients-far better than using your own bone.
What Happens After Surgery?
Recovery isn’t quick. You’ll need 6 to 8 weeks of restricted activity-no lifting, twisting, or bending. Physical therapy starts around 6 weeks out and lasts 3 to 6 months. Full healing? That can take 12 to 18 months.Success rates are high-78-85% of patients report being satisfied at the 2-year mark. But there’s a catch: about 12-15% of people with high-grade slips need another surgery later. Why? Adjacent segment disease. The spine above or below the fused area starts to wear out faster because it’s taking on extra stress. About 1 in 5 people develop this within five years.
That’s why patient selection matters more than ever. A 2023 study identified 11 specific signs-like disc height loss, facet joint arthritis, and nerve compression patterns-that can predict who will benefit from fusion with 83% accuracy. If your doctor doesn’t use these tools to guide the decision, ask why.

Are There Alternatives to Fusion?
Yes-but they’re not for everyone. Motion-preserving devices, like dynamic stabilization systems, use flexible rods to limit movement without fully fusing the spine. They’re being used more often for Grade I-II slips, especially in younger patients who want to keep some flexibility.Early data shows 76% success over five years. That’s good, but still lower than fusion’s 88%. And long-term data? Still limited. These devices aren’t approved for high-grade slips or cases with severe nerve compression.
Stem cell therapies and platelet-rich plasma (PRP) are being studied, but right now, there’s no strong evidence they fix spondylolisthesis. Don’t waste money on unproven treatments.
When to Seek Help
If you’ve had lower back pain for more than 3-4 weeks that doesn’t improve with rest, or if you’re starting to feel numbness, tingling, or weakness in your legs, see a doctor. Don’t wait until you can’t walk. Early diagnosis means better options.And if you’re a parent and your child has persistent back pain after playing sports? Get it checked. Spondylolisthesis shows up in kids as young as 6, especially if there’s a family history. Early intervention can prevent progression.
Can spondylolisthesis get worse over time?
Yes, especially if it’s degenerative or high-grade. Without treatment, the slip can progress slowly over years, especially with continued stress on the spine. But many people’s condition stays stable for decades with proper activity management and core strength.
Is walking bad for spondylolisthesis?
Not always. Short, paced walks are often recommended as part of therapy. But long walks or standing for hours can trigger pain, especially with a high-grade slip. Using a cane or walker for support can help. If walking hurts, stop and rest. Don’t push through it.
Does spondylolisthesis qualify for disability?
It can, if it severely limits your ability to work. The key is documentation: imaging, pain logs, therapy records, and doctor statements showing you’ve tried all conservative options and still can’t perform basic job functions. Many people get approved after fusion if they still have nerve pain or mobility issues.
Can I still exercise with spondylolisthesis?
Absolutely-but not all exercises are safe. Avoid heavy lifting, back extensions, and high-impact sports. Focus on swimming, stationary biking, and core-strengthening moves like bird-dogs and dead bugs. A physical therapist can design a safe program for you.
Will I need a back brace after fusion?
Sometimes, especially if the fusion is in the lower spine or if you’re older or have weak bones. Most surgeons use braces for 6-12 weeks to support healing. But with modern screws and interbody cages, many patients don’t need one at all. It depends on your case.
Final Thoughts
Spondylolisthesis isn’t a death sentence. It’s not even always a problem. For many, it’s just a quiet fact of aging-like gray hair or needing reading glasses. But when it causes pain, mobility loss, or nerve damage, it’s time to act.The best outcomes come from early diagnosis, honest conversations with your doctor, and sticking with rehab-even when it’s boring. Surgery works well for the right people, but it’s not a magic fix. Recovery takes patience. And the most important thing? Don’t ignore persistent back pain. Get it checked. Your spine will thank you.


8 Comments
astrid cookJanuary 26, 2026 AT 15:37
I've seen so many people ignore this until they can't walk. My sister waited two years because she thought it was just 'old age'-then she ended up in a wheelchair for three months. Doctors didn't even mention fusion until she was in crisis. Stop normalizing pain. Your spine isn't a suggestion box.
And if you're still doing yoga twists or deadlifts? You're not strong-you're reckless.
Marian GilanJanuary 28, 2026 AT 09:13
so u know what they dont tell u? the real cause? 5g towers and the chemtrails messing with our bone density. i mean, why else would only americans get this? and why do all the docs say 'wear a brace' but never ask if u live near a cell tower? i had this after my phone died for 3 days and my back felt better. coincidence? i think not.
also, fusion is just the gov'ts way to keep u dependent on opioids and titanium. they make more money off u broken than u fixed. ask why the FDA banned natural bone stimulators but approved bmp-2. hmm?
Paul TaylorJanuary 28, 2026 AT 17:06
Look I've been working with chronic back pain patients for over 15 years and the biggest mistake people make is thinking the spine is some fragile glass statue that's gonna shatter if you sneeze wrong. It's not. It's a living structure that adapts. The real issue isn't the slip it's the fear around it. People panic when they see 'Grade II' on an X-ray and immediately think surgery or disability. But most of them just need to stop sitting on couches all day and start moving their hips and glutes properly. Core strength isn't about six packs it's about stability. And yeah I know PT is boring but if you do 15 minutes a day for three months you'll be walking without wincing. The problem isn't the spine it's the mindset. We treat backs like they're broken toys instead of muscles that just need to be used right.
Also stop blaming everything on smoking or weight. I've had patients who were 180 pounds and never smoked and still had zero pain with proper movement. And I've had lean runners with Grade III slips who were fine because they didn't arch their backs every time they lifted a coffee cup. It's not the slip it's the movement pattern.
Murphy GameJanuary 29, 2026 AT 09:47
They're lying about fusion success rates. I read the 2023 study they cited-it was funded by Medtronic. The '83% accuracy'? That was based on data from patients who already had insurance-approved surgery. What about the ones who couldn't afford it? Or the ones who got denied? They don't count those. And the 12-15% needing revision surgery? That's not 'adjacent segment disease' that's the hardware failing because they used cheap screws and rushed the procedure. I know a guy who had a TLIF and ended up with a nerve that felt like it was being electrocuted every time he sat down. They told him it was 'normal post-op sensation'. Bullshit.
And don't even get me started on BMP-2. That stuff causes swelling the size of grapefruits. One patient I know had to be rushed to the ER because his throat swelled shut. They call it 'a rare side effect'. I call it a cover-up.
John O'BrienJanuary 30, 2026 AT 16:08
Bro I had this and I didn't know it for 4 years. Thought I was just out of shape. Then one day I couldn't get out of my car without screaming. PT saved me but only because my therapist didn't give me the usual 'do squats' crap. She taught me how to brace my core like I was about to get punched in the gut. That's it. No magic. Just learning how to not collapse when you stand. And yeah I quit smoking. No excuses. If you're still smoking and you have back pain you're not trying.
Also if you think walking is bad you're wrong. I walk 8K steps a day now. I just don't drag my feet. I roll through my hips. It's like walking like a ninja. Not a zombie. Try it.
Andrew ClausenJanuary 31, 2026 AT 16:32
The Meyerding scale is not a diagnostic tool-it's a classification system. Misrepresenting it as a predictor of surgical necessity is misleading. Furthermore, the claim that '80% of cases improve with conservative care' is statistically misleading without specifying the time frame, definition of 'improve,' and control variables. The referenced 2023 study on fusion prediction accuracy was retrospective and contained selection bias. The use of BMP-2 is not universally approved; it carries black box warnings for ectopic bone formation and increased cancer risk in certain populations. The assertion that 'no strong evidence exists' for PRP or stem cells is outdated; multiple randomized controlled trials published in 2024 show modest but statistically significant pain reduction in Grade I-II cases. To dismiss these as 'unproven' is irresponsible. The article reads like a pharmaceutical whitepaper disguised as patient education.
Candice HartleyFebruary 1, 2026 AT 02:59
My grandma had this and never told anyone. She just leaned on the counter while cooking. 😔 I didn't realize until she couldn't stand to hug me anymore. I wish I'd known sooner. I'm getting checked now. 💙
Harry HendersonFebruary 2, 2026 AT 01:53
STOP WAITING. If your hamstrings feel like they're glued to your spine, you're not 'just stiff'-you're one step away from being sidelined for good. I was a firefighter. I thought I was tough. Then I couldn't climb stairs without stopping. Did PT. Did the boring stuff. Did it for 6 months. Now I hike 10 miles on weekends. Your spine doesn't care how hard you lift. It cares if you move right. Move. Now. Don't text. Don't scroll. Get up. Stretch. Walk. Do the bird-dog. Right now. I'm not asking. I'm telling you. Your future self is begging you.