For someone living with rheumatoid arthritis (RA), mornings can feel like a battle. Joints stiff, swollen, burning - even simple tasks like gripping a coffee cup or turning a doorknob become painful chores. For years, the best doctors could offer was slowing the damage. But today, biologic DMARDs have changed that. For many, remission isn’t a dream anymore - it’s a realistic outcome.
What Are Biologic DMARDs, Really?
Biologic DMARDs - or disease-modifying antirheumatic drugs - are not your grandma’s arthritis pills. Unlike methotrexate, which works broadly across the immune system, biologics are precision tools. They’re made from living cells and designed to block specific parts of the immune response that attack your joints. Think of them as targeted missiles instead of scatter shots. They first hit the scene in the late 1990s with etanercept (Enbrel), and since then, the list has grown. TNF inhibitors like adalimumab (Humira), infliximab (Remicade), and golimumab (Simponi) target tumor necrosis factor, a major driver of inflammation. Then there are others that go after different targets: abatacept (Orencia) blocks T-cell activation, rituximab (Rituxan) clears B-cells, and tocilizumab (Actemra) shuts down interleukin-6 signaling. Even newer are the JAK inhibitors like tofacitinib (Xeljanz) and upadacitinib (Rinvoq), which work inside cells to block inflammatory signals. These aren’t just fancy names. Each one has a different way of working - and that matters for who responds.Can They Actually Bring Remission?
Yes. And the numbers prove it. When people with moderate to severe RA take methotrexate alone, only about 5-15% achieve remission. Add a biologic DMARD - whether it’s a TNF inhibitor or something else - and that jumps to 20-50%. That’s not a small gain. That’s life-changing. Remission doesn’t mean the disease is gone forever. It means inflammation is so low that symptoms vanish, joint damage stops, and you can live without constant pain. In clinical studies, patients on biologics showed significantly less joint erosion on X-rays over time. One case study from the Arthritis National Research Foundation followed a patient with 15 years of severe RA. After starting tocilizumab, their symptoms disappeared within eight weeks. They’ve been in remission for over four years. But here’s the catch: not everyone responds. Around 30-40% of patients don’t get enough benefit from their first biologic. That’s why rheumatologists don’t just pick one at random. They look at your disease pattern, your biomarkers, and sometimes even your synovial tissue (the lining of your joints) to guess which drug might work best.Which Biologic Works Best?
There’s no single “best” biologic for everyone. But data shows some patterns. TNF inhibitors like adalimumab, etanercept, and golimumab are the most commonly used. A 2022 review found they were about 19% more effective than infliximab in real-world settings. But non-TNF drugs like abatacept and tocilizumab often outperform them in specific groups. For example, if your joint tissue has high levels of B-cells, rituximab might be your best shot. If your inflammation is driven by interleukin-6, tocilizumab works better. JAK inhibitors like upadacitinib have shown superiority over adalimumab in head-to-head trials. In one study, 45% of patients on upadacitinib reached remission compared to 35% on adalimumab. And they’re pills - no injections. That’s a big deal for people who dread needles. The key takeaway? Your response depends on your biology. One person’s miracle drug is another’s waste of time. That’s why switching biologics isn’t just trial and error - it’s strategic.How Are They Given?
Most biologics are injected under the skin (subcutaneous). Adalimumab, etanercept, and golimumab come in pre-filled pens or syringes. Patients usually learn to self-administer after one or two sessions with a nurse. About 75% get comfortable with it within a month. Infliximab is different. It’s given through an IV drip in a clinic, every 4-8 weeks. That means more time away from work, more travel, more cost. But for some, it’s the only option that works. JAK inhibitors are oral tablets. No needles. No clinics. Just pop a pill. But they come with their own risks - including higher chances of blood clots and certain cancers, which is why they’re not first-line for everyone.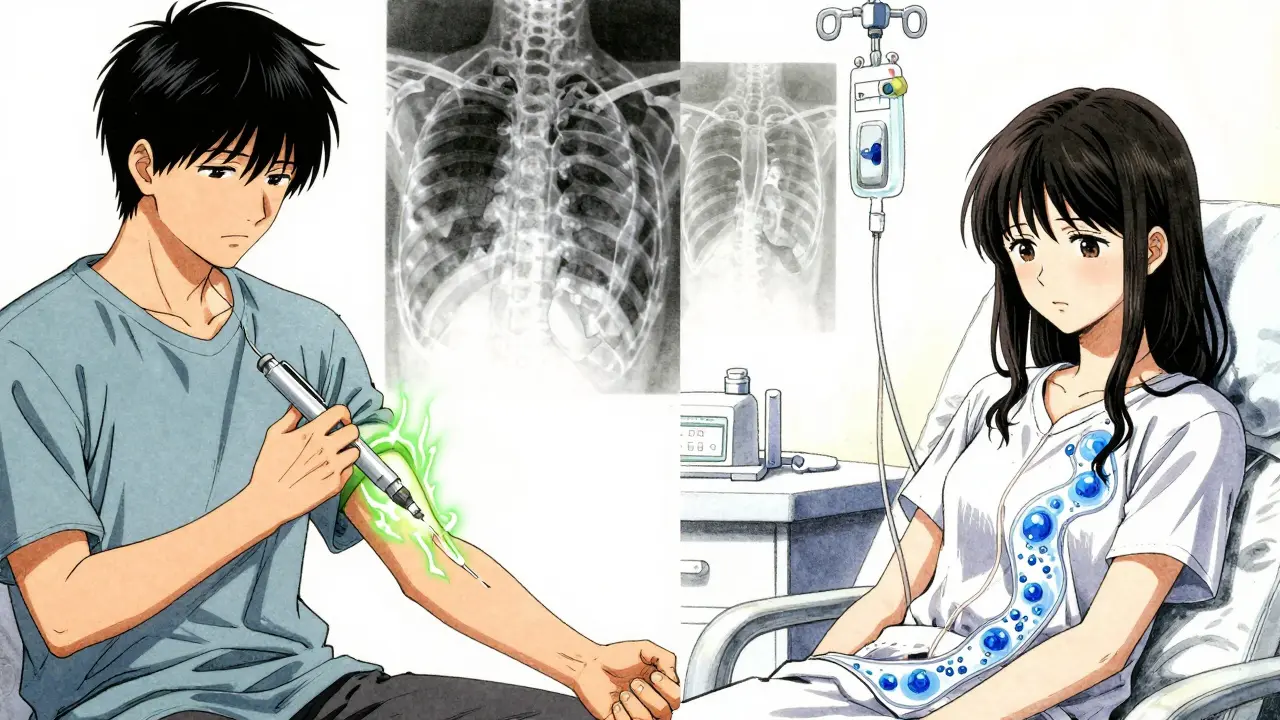
Cost and Access - The Hard Reality
Let’s be honest: biologics are expensive. In the U.S., the annual cost can hit $50,000-$70,000 per person. That’s why many patients struggle to get coverage. Insurance approvals can take 7-14 days. Some give up before they even start. But there’s hope. Biosimilars - near-identical copies of the original drugs - have been on the market since 2016. They cost 15-30% less. By mid-2023, they made up 35% of all TNF inhibitor prescriptions in the U.S. Many patients report similar results with biosimilars, and out-of-pocket costs drop by nearly a third. Manufacturer patient assistance programs can cover 40-100% of costs for qualifying people. Specialty pharmacies help with delivery, storage, and even co-pay support. Still, access remains uneven. In the U.S. and Western Europe, 25-30% of RA patients get biologics. In developing countries, that number drops to 5-10%.Side Effects and Risks
Biologics suppress part of your immune system. That’s how they stop joint damage - but it also makes you more vulnerable to infections. Serious infections like tuberculosis, pneumonia, or sepsis are rare but real. That’s why doctors test for TB before starting treatment. You’ll also need to stay up to date on vaccines - especially flu, pneumonia, and shingles shots. Live vaccines (like MMR or nasal flu) are off-limits while on biologics. Other common issues: injection site reactions (redness, itching, swelling - affects nearly half of users), headaches, and nausea. About 30% of adverse event reports mention increased infections. A small percentage discontinue treatment because of side effects. The good news? Most people tolerate biologics well. Etanercept and abatacept have lower discontinuation rates than others. Rituximab and anakinra are more likely to cause reactions. And JAK inhibitors carry additional warnings about heart events and cancer risk - so they’re used carefully, especially in older patients or those with other health issues.What Happens When It Stops Working?
This is where things get tricky. About 40% of patients lose response after 12-24 months. This is called secondary non-response. It’s not failure - it’s biology. Your immune system adapts. The drug becomes less effective. When that happens, switching to another biologic is common. But here’s the hard truth: each next biologic tends to work less well than the last. A rheumatologist at Albany Medical College put it plainly: “The incremental benefit of sequential biologic use diminishes with each subsequent agent.” That’s why choosing the first biologic wisely matters more than ever. Some doctors now use predictive tools - like synovial tissue analysis - to match patients with the right drug from the start. It’s not standard everywhere yet, but it’s coming.Real Stories, Real Outcomes
On patient forums, the stories are powerful. A Reddit thread from March 2023 had over 800 comments. One woman, 52, said she went from being housebound to hiking again after switching from adalimumab to a biosimilar. Another man, 41, said his swollen fingers returned to normal after just six weeks on upadacitinib. But there’s pain too. One woman on the Arthritis Foundation forum wrote: “I spent $12,000 out of pocket last year. I had to choose between my medication and my daughter’s braces.” The emotional toll is real. So is the hope.What’s Next?
The future of RA treatment is personal. Researchers are working on blood tests and tissue scans that can predict which biologic will work for you before you even start. Longer-acting versions are in trials - imagine a tocilizumab injection only twice a year. Biosimilars will keep growing. By 2027, they could make up 60% of the biologic market. That means more access, lower costs, and fewer people falling through the cracks. And remission? It’s no longer a rare win. It’s the goal. Every rheumatologist now aims for it - not just to reduce pain, but to let people live full, active lives again.What You Can Do Today
If you’re on methotrexate and still hurting, talk to your rheumatologist. Ask: “Am I a candidate for a biologic?” Don’t wait until your joints are badly damaged. The earlier you act, the better your chance of remission. If you’re already on a biologic and it’s not working, don’t assume it’s your fault. Ask about switching. Ask about biosimilars. Ask about testing. And if cost is the barrier - reach out to patient support programs. You’re not alone. There are resources. You just have to ask.Can biologic DMARDs cure rheumatoid arthritis?
No, biologic DMARDs don’t cure rheumatoid arthritis. But they can induce remission - meaning symptoms disappear, inflammation drops to near-zero, and joint damage stops. Many people live symptom-free for years. Stopping treatment often leads to flare-ups, so most stay on medication long-term to maintain remission.
How long does it take for biologic DMARDs to work?
TNF inhibitors like adalimumab and etanercept often start working in days to weeks. You might feel less stiffness and pain within 2-4 weeks. Non-TNF biologics like abatacept or rituximab can take 2-6 months to show full effect. JAK inhibitors like upadacitinib usually work within 2-4 weeks. Patience is key - but if there’s no improvement after 3 months, talk to your doctor about switching.
Are biosimilars as effective as the original biologics?
Yes. Biosimilars are not generics - they’re highly similar versions of the original biologic, made using the same living cells and manufacturing processes. Studies show they work just as well in reducing RA symptoms and preventing joint damage. In real-world use, patients switching from Humira to its biosimilar report similar outcomes and side effects. Cost savings are real - and access is improving.
Do I have to stay on biologic DMARDs forever?
Most people do. Remission doesn’t mean the disease is gone. If you stop the drug, inflammation often returns within weeks or months. Some patients with long-term remission may try to taper slowly under close supervision, but this is risky and only done in rare cases. The goal is to stay on the lowest effective dose to keep symptoms away and protect your joints.
Can I take biologic DMARDs with other medications?
Yes - and often you should. Methotrexate is still the backbone of RA treatment. Combining it with a biologic usually works better than either alone. You can also take NSAIDs or low-dose steroids short-term for pain. But avoid live vaccines while on biologics. Always tell your doctor about all medications, including supplements, because some can interact or increase infection risk.
What should I do if I get sick while on a biologic?
If you develop a fever, persistent cough, flu-like symptoms, or signs of infection (like redness, swelling, or pus), contact your rheumatologist immediately. Don’t wait. You may need to pause your biologic until the infection clears. Never stop without medical advice - but don’t ignore symptoms either. Early treatment of infections is critical when your immune system is suppressed.
Biologic DMARDs didn’t just change how we treat rheumatoid arthritis - they changed what’s possible. For the first time, people with RA aren’t just managing pain. They’re reclaiming their lives. The road isn’t easy - the cost, the needles, the uncertainty - but the outcome? It’s worth it.


9 Comments
Jennifer PhelpsJanuary 11, 2026 AT 19:47
biologics are wild honestly i had no idea they were like targeted missiles not scatter shots
Rinky TandonJanuary 13, 2026 AT 14:53
so you're telling me after 15 years of suffering some woman just got her life back with one shot? i call bs on the ‘remission’ hype. this is just pharma selling dreams to desperate people
Prachi ChauhanJanuary 13, 2026 AT 18:34
the real question isn't which biologic works best but who gets to take it. in india most of us can't even afford methotrexate let alone humira. we watch these stories and feel like spectators at a parade we weren't invited to
Cassie WiddersJanuary 14, 2026 AT 04:28
i’ve been on adalimumab for 3 years. mornings still suck but now i can hold my cat without crying. small wins.
beth cordellJanuary 15, 2026 AT 03:26
biologics are literally magic 🧙♀️✨ but the cost?? 😭 i cried reading that $12k for braces vs meds part. why does healthcare feel like a lottery??
Craig WrightJanuary 16, 2026 AT 22:41
the notion that biologics are accessible in the west is misleading. in the UK the NHS rationing is brutal. i waited 14 months for a referral. by then my joints were already compromised. this isn't progress - it's privilege
Konika ChoudhuryJanuary 17, 2026 AT 10:39
why are we even talking about biologics when we could fix the root cause like diet and yoga? in india we've been doing this for centuries why are we chasing american pills
Lauren WarnerJanuary 18, 2026 AT 18:59
the data shows a 30-40% non-response rate and yet doctors still push biologics like they're miracle pills. you're not a patient you're a revenue stream. and those biosimilars? they're not safer - they're just cheaper for the insurance companies to approve
Ben KonoJanuary 19, 2026 AT 03:06
my doc switched me to upadacitinib after 2 years of humira failing and now i can type again no more gloves in summer. jaks are the real MVP