Pediatric Medication Safety Calculator
WARNING: Never give adult medications to children, even in reduced doses. Always use pediatric-specific formulations.
Medication Information
Child Information
Calculated Dose
Based on your child's weight and the medication concentration
Every year, 50,000 children under age 5 end up in emergency rooms because they got into medicine they shouldn’t have. Many of these cases aren’t accidents-they’re preventable mistakes rooted in assumptions that work for adults but are deadly for kids. Children aren’t just small adults. Their bodies process medicine differently, they can’t tell you when something feels wrong, and even a tiny mistake in dosage can turn a lifesaving drug into a lethal one.
Why Kids Are at Higher Risk
Children’s bodies are still growing. Their kidneys and liver, the organs that break down and flush out medicine, aren’t fully developed. That means even a correct dose for an adult could build up to toxic levels in a baby. A 2-year-old weighing 12 kilograms needs a completely different amount than a 14-year-old weighing 60 kilograms. That’s a five-fold difference in body weight-and if you get the math wrong, you’re not just off by a little. You’re off by a life-threatening amount.One of the most common errors? Mixing up teaspoons and milliliters. A teaspoon holds 5 milliliters. If a parent gives 1 teaspoon thinking it’s the same as 1 milliliter, they’ve just given a five-times overdose. That’s not rare. It happens every day. And it’s not just about liquid meds. Pills, patches, eye drops-even vitamins and diaper rash cream-can kill a child if they get into them.
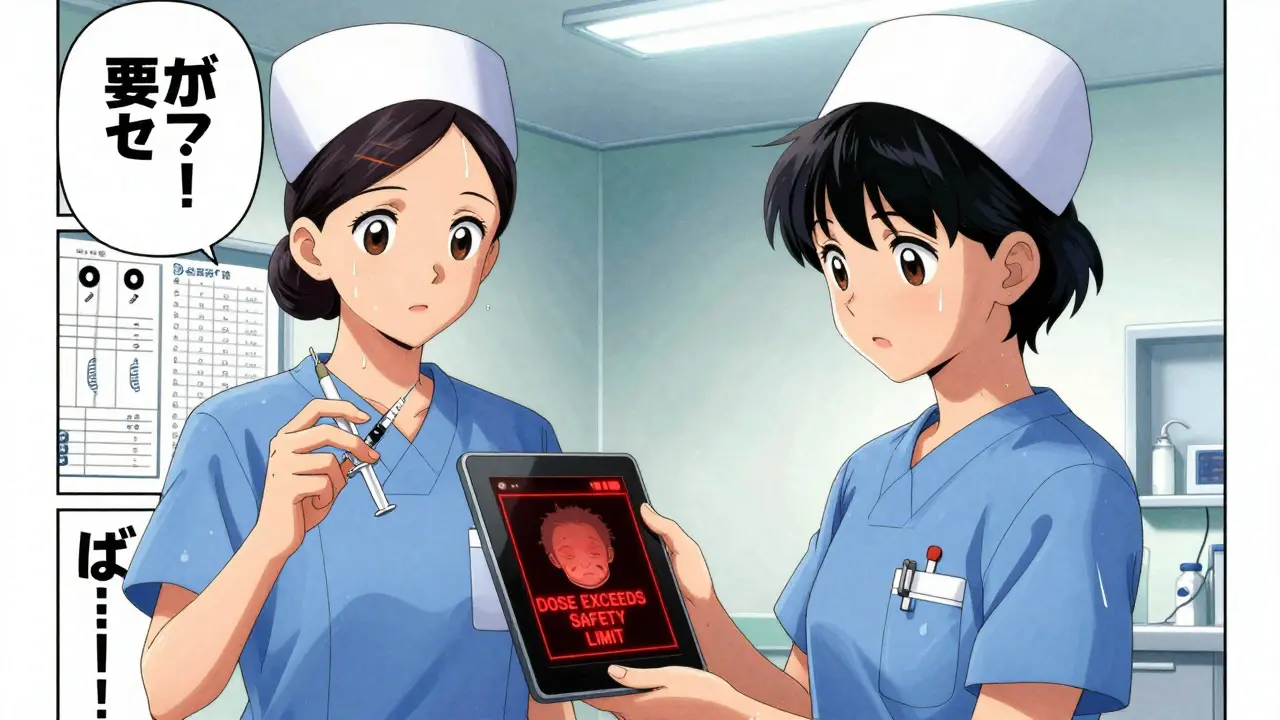
What Happens in Hospitals
In hospitals, pediatric medication errors are the leading cause of serious harm. The Joint Commission reports that 42% of all serious pediatric medication incidents are caused by weight-based dosing mistakes. That’s because many hospitals still use pounds instead of kilograms when calculating doses. One wrong decimal point, one misread number, and you’ve got a child on the wrong dose.Top children’s hospitals now use strict rules to stop this:
- Weight must be entered and calculated only in kilograms
- Electronic systems block doses above safe upper limits
- High-risk drugs like morphine or insulin are prepared in distraction-free zones
- Two trained staff members independently check every dose before giving it
These aren’t suggestions-they’re now standard practice in over 78% of children’s hospitals following the 2018 American Academy of Pediatrics guidelines. But in general hospitals with fewer than 100 pediatric patients a year, error rates are 3.2 times higher. Why? Because staff aren’t trained often enough. They don’t see kids often. And they don’t have the systems built for them.
Home Medication Mistakes Are Even More Common
Most pediatric poisonings happen at home. Not in the ER. Not in the pharmacy. In the kitchen cabinet. On the nightstand. In the purse.The CDC’s PROTECT Initiative found that 75% of children who get into medicine do so from storage locations their parents thought were “safe.” A locked cabinet? Great. But if it’s at eye level, or if the child climbed on a chair to reach it, it’s not safe. A study showed kids can open a child-resistant cap in under 30 seconds if it’s not fully clicked shut.
And it’s not just pills. Parents don’t think of cough syrup, eye drops, or prenatal vitamins as dangerous-but they are. One pill of a heart medication can stop a baby’s heart. A few drops of an opioid patch can cause breathing to stop. Even a single chewable vitamin with iron can cause organ failure in a toddler.
What You Should Never Do
There are simple rules that can save a child’s life:- Never call medicine “candy.” Saying “this will taste sweet” or “it’s like gummy bears” teaches kids to seek out pills. That’s why 15% of accidental ingestions come from children who think medicine is food.
- Never use kitchen spoons to measure medicine. A teaspoon from your drawer holds anywhere from 3 to 7 milliliters. Always use the dosing cup, syringe, or dropper that came with the medicine.
- Never give cough or cold medicine to kids under 6. The FDA and American Academy of Pediatrics agree: these drugs don’t work for young kids and carry serious risks. The same goes for kids under 2-no exceptions.
- Never leave medicine out. Even if you’re just going to the bathroom. Even if you think your child can’t reach it. A child can climb, crawl, or pull down a bag in less than a minute.
How to Store Medicine Safely at Home
Safe storage isn’t about locking it up-it’s about making it impossible for a child to find or reach.- Store all medicine, including vitamins and topical creams, up and away-not on counters, nightstands, or in purses.
- Use locks on cabinets. But don’t rely on child-resistant caps alone. They’re not child-proof-they’re child-resistant. And if they’re not snapped shut, they’re useless.
- Keep a list of all medicines in the house, including what’s in the bathroom, garage, or car. Check it monthly.
- Dispose of old or expired medicine properly. Don’t flush it. Don’t throw it in the trash. Take it to a pharmacy drop-off or a community disposal event.
How to Give Medicine Correctly
When it’s time to give medicine, follow these steps:- Check the label. Is it the right name? Right dose? Right child?
- Use the device that came with the medicine. If it’s a syringe, use the syringe. If it’s a cup, use the cup.
- Give the dose slowly, aiming toward the back of the cheek-not the tongue. This helps avoid choking and ensures the full dose is swallowed.
- Write down what you gave and when. Use a chart or phone app. If you’re tired or stressed, you’ll forget.
- Ask the pharmacist: “Is this safe for my child’s age and weight?” If they don’t know, get a second opinion.
Studies show that using pictogram-based instructions-simple pictures showing when and how to give medicine-improves correct dosing by 47% in families with low health literacy. Ask for them. They’re free.
Teach Your Child About Medicine
Kids learn by watching. If they see you take medicine every day, they’ll want to do it too. That’s normal. But you can turn that curiosity into safety.- Teach them: “This is medicine. It helps grown-ups feel better. It’s not candy.”
- Keep medicine out of sight and reach-even when you’re home.
- If you use a pill organizer, keep it locked or in a high drawer.
- Don’t leave medicine in the car. Kids see it. They think it’s okay.

What to Do If a Child Gets Into Medicine
If you think your child swallowed medicine, don’t wait. Don’t call your doctor first. Don’t Google symptoms. Don’t try to make them throw up.Call Poison Control immediately: 800-222-1222. That number should be saved in every phone in your house. Program it into your cell, your landline, your smart speaker. Keep it on the fridge.
Have this ready when you call:
- What the child swallowed
- How much
- When
- How old they are
- How much they weigh
Even if they seem fine, call. Some drugs take hours to show effects. And poison control experts know exactly what to do. They’ve seen it all.
What’s Changing in 2026
New rules are coming. The FDA now requires all new pediatric medications to come in standardized concentrations. That means no more “10 mg/mL” and “50 mg/mL” versions of the same drug. Just one. Fewer chances for mix-ups.Pharmacies are also starting to dispense liquid medicines only in milliliters-with no teaspoons or tablespoons on the label. And more hospitals are training all staff-not just pediatric teams-on how to safely handle kids’ meds.
But the biggest change? Awareness. More parents are learning that medicine isn’t just something you take. It’s something you protect.
Can I give my child adult medicine if I cut the dose in half?
No. Adult medications are formulated for adult bodies. Even if you cut the dose, the inactive ingredients, absorption rates, and release mechanisms aren’t designed for children. This can cause unexpected side effects, toxicity, or no effect at all. Always use medicine made for children and follow the label or your doctor’s instructions.
Why are pediatric dosing charts based on weight and not age?
Two children of the same age can weigh very different amounts. A 3-year-old might weigh 10 kg, while another might weigh 20 kg. Dosing by weight ensures the right amount of medicine reaches their bloodstream. Age is a rough guide, but weight is the only accurate way to calculate safe doses.
Are over-the-counter medicines safer for kids?
No. Just because a medicine doesn’t need a prescription doesn’t mean it’s safe for children. Many OTC cold and cough medicines have been linked to serious side effects in kids under 6. Even children’s acetaminophen can cause liver damage if given too often or in the wrong dose. Always check the label and talk to your doctor before giving any OTC medicine to a child under 6.
What should I do if my child spits out or vomits medicine?
Don’t give another dose unless you’re sure the full amount was spit out. If you’re not sure, call your doctor or Poison Control. Giving a second dose too soon can lead to overdose. Some medicines stay in the system longer than you think, and doubling up can be dangerous.
Is it safe to crush pills or open capsules for my child?
Only if your doctor or pharmacist says it’s okay. Many pills are designed to release medicine slowly. Crushing them can cause the full dose to be released at once, which can be dangerous. Some capsules contain powders that are harmful if inhaled. Always ask before altering the form of any medicine.


11 Comments
Alec AmiriJanuary 22, 2026 AT 23:18
My cousin’s kid swallowed half a bottle of children’s Tylenol last year. She thought ‘one teaspoon’ meant one spoon from the kitchen. Turns out that’s like 3500mg. Kid ended up in ICU for 4 days. Don’t be that parent. Use the damn syringe.
And stop calling medicine candy. I swear, every time I hear a mom say ‘this is like gummy bears’ I want to scream.
It’s not cute. It’s a death sentence waiting to happen.
Daphne Mallari - TolentinoJanuary 23, 2026 AT 02:18
While the article presents a compelling case for standardized pediatric dosing protocols, it is regrettable that such basic pharmacological principles remain unenforced in domestic settings. The reliance on parental discretion-particularly in households lacking formal medical training-constitutes a systemic failure in public health infrastructure. The FDA’s forthcoming standardization initiative is a necessary, albeit overdue, corrective measure.
Neil EllisJanuary 23, 2026 AT 04:43
I love how this post doesn’t just scare us-it gives us a roadmap. Like, imagine if every kitchen had a little sticker on the cabinet that said ‘Medicine = Not Candy’ in big letters. Or if pharmacies handed out those pictogram cards like they were free candy.
My aunt used to keep her meds in a little wooden box on the counter. Said it was ‘for easy access.’ I used to sneak in and count the pills like they were marbles. She never knew.
Now she keeps them locked up, high up, and labeled with pictures. And guess what? Her grandkids never even ask. They just know. That’s the magic right there.
Let’s make safety normal, not scary. Let’s make it beautiful. Let’s make it stick.
Ryan RiestererJanuary 25, 2026 AT 03:14
The 42% figure cited from The Joint Commission is corroborated by the 2020 NEJM study on pediatric dosing errors in mixed-use hospitals. The primary confounding variable remains the use of imperial units in weight documentation. Kilograms are not merely preferable-they are non-negotiable in clinical contexts. The 3.2x higher error rate in low-volume pediatric settings aligns with cognitive load theory: infrequent exposure reduces procedural fluency, increasing reliance on heuristic-based dosing, which is inherently error-prone.
Additionally, the omission of pharmacokinetic variability across developmental stages (e.g., neonatal CYP450 immaturity) in public messaging is a critical gap. Parents need to understand that metabolism isn’t linear with size-it’s ontogenetic.
Sarvesh CKJanuary 26, 2026 AT 22:13
It is fascinating to observe how deeply cultural attitudes toward medicine shape safety outcomes. In my home country, India, many families keep medicines on shelves near children’s toys, believing that ‘if it’s in the house, it’s meant to be used.’ There’s also a strong tradition of self-medication based on family wisdom-‘my sister gave her child this for fever, it worked.’ This creates a dangerous normalization of risk.
Yet, I’ve seen communities in Kerala change this through simple visual posters in local temples and schools-showing a child reaching for a bottle with a red X. No words needed. Just images. And within a year, ER visits for pediatric ingestions dropped by 40%.
Perhaps the solution isn’t more rules, but more storytelling. More shared human experiences. More silence around judgment, and more space for compassion and learning.
Hilary MillerJanuary 28, 2026 AT 16:39
My kid opened a child-resistant cap in 12 seconds. I was stunned. Then I cried. Now everything’s locked. No excuses.
Margaret KhaembaJanuary 28, 2026 AT 19:27
So… what about vitamins? I always thought those were harmless. But now I’m paranoid. Is a single chewable iron vitamin really that dangerous? My 2-year-old loves those gummy ones. 😅 Should I just stop giving them? Or is it safe if they’re locked up?
Malik RonquilloJanuary 30, 2026 AT 09:16
Why do we even need a 2000-word essay to tell people not to leave pills lying around
It’s 2025. Not 1985. If you can’t keep your meds out of reach, maybe you shouldn’t have kids
Brenda KingJanuary 31, 2026 AT 17:19
Thank you for writing this. I needed this. I used to keep my meds in my purse. My daughter is 3 now. She pulled out my blood pressure pill once. I didn’t even notice until she was chewing it. I screamed. She laughed. Now everything’s locked. High. And I use the syringe. Always. I’m so glad I read this. ❤️
Keith HelmFebruary 2, 2026 AT 10:05
Kindly clarify whether the 78% adoption rate of AAP guidelines includes outpatient clinics or solely inpatient pediatric units. Additionally, please provide the source of the 47% improvement statistic regarding pictogram-based instructions.
Patrick RothFebruary 2, 2026 AT 23:11
Actually, the real problem is that we’ve turned medicine into this terrifying monster. Kids are curious. That’s how they learn. Locking everything up just makes it more fascinating. What if we taught them *why* it’s dangerous instead of treating them like little thieves?
And who says teaspoons are wrong? My grandpa measured everything by teaspoons. Never had a problem. Maybe we’re over-engineering this.